Leykhtenstern so kot razlog za invaginacije poškodb navedene tudi akutne bolezni, neposredno predšestvovavsh s črevesnimi izvedbami (na primer poškodbe trebušne stene, ponosa, prehlad in tako naprej), in kronično potekajoče bolezni. (raki, polipi, itd.), vendar očitno prevladuje pomanjkanje kakršnih koli navodil v anamnezi o primerih invaginacije pri prej precej zdravih osebah. Od prejšnjih kroničnih bolezni je treba izpostaviti:1) kronični kolitis, 2) kronične črevesne razjede (tuberkuloza) 3) slepiča, 4) kronične vnetne infiltrate v debelini črevesnih sten, 5) tumorje (raki, sarkomi, epiteliomi, adenomi). , lipomi, miomi, fibromi, miksofibromi, papilomi, angiomi, ciste in druge novotvorbe), 6) strikture, 7) črvi.
Ob pozorni anamnezi lahko registracija teh bolezni seveda prinese nekaj koristi, usmerjeno raziskovanje na pravi način; vendar v mnogih primerih invaginacije oddaljena anamneza ne daje ničesar, saj se izvajanje dogaja na tleh različnih prirojenih predispozicij in zgolj iz za zdaj neznanih razlogov. Sklicujte se na število anomalij, ki prispevajo k izvajanju, kot vemo, podaljšanje mezenterijev, gibljivost slepega črevesa (obstoj mezokoekuma), mekkeljeve divertikule, izbokline v bleščici slepo črevo bauginijevih vrat in tako naprej.
Te anomalije je skoraj nemogoče razlikovati v pogojih nujnega kirurškega posega.
Poleg naštetih kroničnih bolezni je treba pri zbiranju anamneze na daljavo upoštevati še vse prejšnje operacije. Pri njihovem ocenjevanju je treba upoštevati, da so v zadnjem času pogosteje opisani primeri črevesnih invaginacij v želodcu po različnih gastroenterostomijah:zadaj, spredaj, s kratkimi zankami, z dolgimi, z interintestinalno anastomozo in brez njih; poleg tega so takšne črevesne invaginacije opisane tudi po resekciji želodca. Prvi primer podobne invaginacije opisuje Steber leta 1917. G. Batman in Baldwin leta 1933 opisuje 33 takih primerov. Leta 1936 je gospod Gottesmen opisal 40 primerov. Pri nas v Zvezi so o teh invaginacijah poročali D. M. Gorodinsky, M. V. Zamoshchin, V. V. Uspensky in V. I. Sokolov, S. S. Penkevich itd. Iz tega seznama sledi, da število podobnih invaginacij raste. Vendar pa V. V. Uspensky in V. I približen izračun. Sokolova, enterogastrične invaginacije se ne pojavljajo pogosteje kot 1 invaginacija na 1500 narejenih gastroenterostomija, vendar se bo očitno z množenjem primerov uvedbe soustije povečalo tudi število invaginacije. Henshin loči naslednje oblike invaginacije jejunuma v želodcu:
M. B. Zamoshchin tej shemi doda še naslednje oblike:
V. V. Uspensky in VI Sokolov, izhajajoč iz že opisanega nadzora, pa tudi iz teoretičnih razlogov, načrtujeta večjo količino oblik podobnih izvedb.
Termin, ki izhaja od trenutka nalaganja anastomoze do oblikovanja izvedbe po različnim avtorjem, znaša od 6 dni do 16 let. Vendar pa so najpogosteje opazili invaginacije v 2. letu pooperativnega toka. Po uvedbi hrbtne soustije se invaginacija pojavi približno 4-krat pogosteje kot po lobiji. Zadnjo okoliščino očitno razlaga dejstvo, da se na splošno hrbtna anastomoza naredi veliko pogosteje kot lobiji.
Kot je bilo že omenjeno, zelo pogosto pride do izvedbe brez vidnih razlogov. Med zadnjimi opisujejo tako telesne kot duševne poškodbe. Komunikacija duševne poškodbe z invaginacijo sestoji iz vpliva prestrašenosti, strahu na peristaltiko, katere krepitev lahko vodi do izvajanja (Vortmann).
Invaginacije zaradi telesne poškodbe so opisane kot po ranah s strelnim orožjem (LA Kirsn er, VN Pavlov-Silvansky, SL Timofeev itd.), in v zvezi z zaprtimi poškodbami trebušne votline iz različnih razlogov.
Izjemno izjemen primer invaginacije po rani od krogle je opisal LA Kirsner.
8/VIII 1920 g bolnika z nenamerno rano v desni polovici trebuha pripeljali v bolnišnico. Rana se je zgodila pred 2 dnevoma. Vhodna odprtina - je 3 prste nižja od popka, 2 cm od povprečne črte; izhod — na sprednji aksilarni liniji, je 3 cm višji od sprednje osi. Rana je potekala skoraj brez gnojenja. Splošno stanje bolnika težko. Pritožuje se zaradi bolečin po vsem trebuhu. Stol po rani ni bil; tudi plini niso odhajali. Želodec je intenziven, v srednjem delu je napihnjen. Območje rane je močno boleče, napeto. Predpostavlja se rana črevesja (slepa), morda od začetka lokalnega peritonitisa.
Naslednji dan v istem stanju, je načrtovano gibanje črevesja; kljub temu ni ne plina, ne stola. Glede na navodilo o lokalni oviri je bilo odločeno za operacijo.
9/VIII operacija (L. A. K in r z N e r) v kloroformni anesteziji. V peritonealni votlini najdemo nekaj strdkov; zanke drobovja so razstreljene in spajkane med seboj; komisure se zlahka ločijo. Skoraj na slepo črevo se odkrije ne povsem jasna izobrazba - tumor, ki doseže velikost skoraj pesti, prilepljen na sprednjo steno želodca. Njegov oddelek se je začel od zgoraj na debelem črevesu, zato je bil močno spremenjen slepo črevo, spajkano na sprednjo trebušno steno želodca, komaj izločen. Glede na to je bila ugotovljena velika napaka serozne ovojnice, ki sega skoraj do mišičnega. Celotna okolica je bila v komisurah in strdkih, po odstranitvi pa je postalo jasno, da gre za vgradnjo ilealnega črevesja v debelo. Narejena je resekcija zadnje zanke ileuma in delov debelega črevesa z implantacijo ileala v križno črevo.
Zadeva je zelo nazorna, jasno kaže vpliv škode.
Pogosteje se pojavljajo enostavnejše poškodbe (modrice, pretres možganov, natuživanje itd.). Mehanizem črevesnih izvedb zaradi poškodb trebušne votline je sestavljen iz primarnega krča poškodovanega dela črevesja, po katerem se izvedba že razvije. Številni avtorji opisujejo krče črevesja zaradi poškodb trebušne votline. Razen poškodb, kot razlog za invaginacije navedite jemanje odvajal, napake v prehrani.
V zadnjem času opišite invaginacije, ki so se pojavile po operacijah. Med tako neštevilnimi nadzori so očitno izpostavljene izvedbe, ki niso povezane z operativnim vplivom. I. L. Bregadze daje naslednji nadzor.
Pacient, 37 let, je bil operiran 13. 11. 1933 v spinalni anesteziji. Narejena je bila resekcija želodca po Billrothovi poti — Hakena — Krenlayna — Eyzelsberg. V pooperativnem obdobju je bilo stanje bolnika ves čas težko. 20/11, torej 7. dan bolezni, je bolnik umrl.
Pri odprtju invaginacije ilealnega in slepega črevesja v naraščajočem debelu z gangrenozno spremembo intususceptuma.
Opisan zanimiv primer pooperativne invaginacije:
A. A. O od l o l in N.
Pacient, 16 let; sredi decembra 1924 je bila opravljena operacija slepiča. Tretji dan po operaciji so po navedbah pacientke bolečine v želodcu, ki niso podobne tistim pred operacijo. Želodec je bil napihnjen. Potem so bolečine nekoliko prenehale, vendar niso izginile. Za 8. dan so šivi odstranjeni, rana se zaceli prva namera, bolnik pa je bil izpisan.
Pacientka navaja, da se je po izstopu iz bolnišnice počutila slabo, saj so se bolečine nadaljevale, ki so občasno dosegle precejšnjo stopnjo, zaradi česar je bila doma prisiljena ležati in nenehno držati termofor. želodec. Zaradi vse večjega poslabšanja je bila sposobna 25. 1. 1925 je pacientka sprejeta v kliniko.
Bolan bled in izčrpan. Temperatura 37,5 °. Pulz 90. Bolni od časa do časa kriči zaradi pojavnih bolečin v trebuhu. Želodec je zmerno napihnjen. Pod popkom na robu desne neposredne mišice operativni rob dolžine 10 cm. Skozi trebušne ovojnice je opazna hrapava peristaltika črevesja. Želodec med napadom bolečine je intenziven, boleč. Pri palpaciji v obdobjih sprostitve trebušne stene na ravni popka je opredeljen upor, ki je navzkrižno in močno boleče kolbasovidno obliko. Pri tolkalih v polju upora je neumen zvok, zgoraj in spodaj - timpaniti. Globlja palpacija želodca v polju upora povzroči močne kontrakcije bolečine. Jezik je moker, ni položen. Bruhanje na dan prejema je bilo 2-krat, stol 3-krat, tekoče, rjave barve. Weberova reakcija na raziskavo kala je zelo pozitivna. Urin:specifična teža - 1024; ne vsebuje beljakovin, sladkorja; mikroskopsko najdemo - 7-10 pregledanih levkocitov, ločenih eritrocitov, celic ravnega epitelija. Levkociti — 13 125. Srce in pljuča brez posebnih sprememb.
Diagnoza – izvajanje črevesja.
Na operaciji je bilo ugotovljeno, da je bil "vpeljan v prečno črevesno slepo, del ascendentnega in ilealnega črevesa, vrh intususceptuma pa je bil definiran na vraničnem kotu debelega črevesa. Resekcija. Okrevanje ". Pri preučevanju zdravila je postalo jasno, "da tisto mesto stene slepega črevesa, kjer je treba invaginirati panj oddaljenega poganjka, ustreza glavici intususceptuma in je precej odebeljeno, debeline 3 cm v prerezu .
Če povzamemo opisani primer, A. A. Ogloblin meni, da se je postopek izvajanja začel 3. dan po operaciji slepiča. Treba se je strinjati z mnenjem avtorja.
Izjemen primer pooperativne invaginacije je bil opažen na kirurškem oddelku bolnišnice Mečnikova.
Pacienta, 46 let, je operiral PN Napalkov 16 /03 1933 glede desne dimeljske kile (pod lokalno anestezijo). Pri odpiranju hernialne vrečke se razkrije, da od vrha tankega črevesa, ki je v vrečki, odstopa nekaj votlih poganjkov (Mekkelov divertikul ali vlečni divertikulum). Poganjek dolžine 5-6 cm in debeline približno kazalca je bil na 3-3,5 cm spojen s hernialno vrečko. Operater je odrezal divertikulum iz črevesne zanke, zašil odprtino v črevesju z torbico in od zgoraj naložil trinadstropne sive in serozne šive. Odrezan poganjk smo odstranili skupaj s hernialno vrečko. Kot posledica odstranitve divertikula v tankem črevesju se je izkazalo vozlasto zadebelitev, ki je nastala zaradi potopitve panja v tobačno vrečko, ki je vstopil v črevesje kot goba. Prehodnost črevesja ni trpela. Hernija je bila zašita na način Ru — Oppelya.
Naslednji dan se je ob 11. uri zvečer pojavila bolečina v bližini popka in kruljenje. Kmalu zatem je razstrelil antikardij, nato pa je prišlo do bruhanja lahke kislinske tekočine. Pulz je bil po tem 90. Ponoči je bolnik spal. Ob svitu je spet bruhalo.
18/03. Zjutraj je spet prišlo do bruhanja. Temperatura 37-37,3 °.
Puls 86. Ni apetita, ne pije. Splošno stanje zadovoljivo. Želodec je rahlo napihnjen, mehak. Zanke črevesja se ne konturirajo.
Ob 8. uri zvečer je spet prišlo do bruhanja:bruhanje kavne barve, kislo, brez vonja. Sifonski klistir ni dal rezultata. Želodec je mehak, vendar malo napihnjen, zanke črevesja se ne konturirujejo. Hude bolečine v popku.
19/III. Temperatura 37,2-38,1 °. Pulz 86. Zjutraj je bilo bruhanje barve kave. Hude bolečine v želodcu, kruljenje, kapotement, peristaltika. Postavi se klistir s terpentinom. Veliko stola, veliko plinov je odšlo. Želodec je padel, bolečine so oslabile. Zvečer ista slika napihnjenosti trebuha, bolečin, vermikuloznega gibanja. Spet je narejen klistir, spet je prišlo do izboljšanja.
20/03. Enako stanje, ista terapija.
21.3. Enako stanje. Klistirji ne delujejo. Ves čas želje na dnu, a neučinkovite. Pulz 86. Temperatura 37 °. Sum na invaginacijo tankega črevesa.
Ob 8. uri zvečer se začne operacija (P. N. Napalkov) pod eterizacijo. Ugotovljena je enterična invaginacija v dolžini 15 cm. Mesto črevesja s pristenochno "gobo" je invaginirano. Izvede se dezinvaginacija in naloži črevesna anastomoza z enostranskim nepopolnim izklopom prizadete zanke. Bolnik je okreval.
Posebno pozornost si zaslužijo invaginacije, ki nastanejo pri bolezni dizenterije in tifusa. Jasno je, da se težave pri prepoznavanju takšnih invaginacij poslabšajo z obstojem osnovne bolezni, katere simptomi zasenčijo znake črevesnega izvajanja. Primer takšne kombinacije dizenterije in invaginacije je lahko eden od nadzorov V. P. Arsenjeva.
Pacient, star 64 let, je prišel iz vasi z ambulantno diagnozo dizenterija. Bolezen je približno 6 dni s krvavo drisko in bruhanjem.
23/VII 1934 g. Temperatura je normalna. Želodec je boleč, mehak, v desni polovici hrapava peristaltika, sondiran je "tumor". Po posvetovanju s kirurgom se bolnik prenese na operacijo v kirurški oddelek. Pred operacijo je bil jasno sondiran tumor, ki zavzema desno ilealno področje. Od časa do časa je bila vidna peristaltika. Stol — sluz s krvjo.
Pri operaciji (pod kloroformom) je bila desna polovica želodca zasedeno napihnjeno ascendentno črevo, v katero so invaginirali slepo in ilealno črevo. Poskus dezinvaginacije ni bil uspešen zaradi hipostaze in obilice komisur. V kloroformni anesteziji se glede na splošno resno stanje in starostne spremembe srca kirurg ni odločil za resekcijo. Naložen je enterokoloanastomoz s prečnim črevesjem. Ves intususceptum je zavit v epiplon in obrobljen s stransko steno.
24. VII. Zdravje je zadovoljivo. Želodec je mehak, rahlo boleč na področju invaginacije. Plini odhajajo, jezik je položen, suh. V pljučih se posluša obilno ropotanje. Do večera je bil samostojen stol s sluzjo in krvjo.
25 in 26/VII. Zdravje je zadovoljivo. Želodec je mehak. driska; koščki sluznice odidejo.
27/VII je prišlo do nenadnega poslabšanja splošnega stanja in bolnik je umrl zaradi pojava peritonitisa, pri temperaturi 36,8-37,8 °.
Odpiranje:močan enterokoloanastomoz, brez pojavov vnetne reakcije; na zadnji steni zunanje cevi intususceptuma - perforativna odprtina na mestu dizenterična razjeda črevesja, velikosti približno pet kopejk; vsa sluznica črevesja je pokrita z dizenteričnimi razjedami; peritonitis.
Mehanizem invaginacije pri griži in tifusu na splošno; tako in druge bolezni v celotnem črevesju so razjede in zlahka pride do krčev, kot tudi tla za pristop izvajanja. Poleg tega je treba upoštevati, da so lahko vzrok za črevesno izvajanje tudi zaužiti tujki in različni črevesni paraziti.
Na splošno se bolniki pri invaginacijah črevesja pritožujejo nad bolečino, ki se pojavi v času izvajanja.
V zgoraj navedenem primeru črevesne invaginacije, ki je zapletla herniotomijo, je bilo mogoče slediti razvoju bolečine iz samega začetka izvajanja in opazovati njegove spremembe v 5 dneh. Pojav bolečin v popkovnem krogu pri črevesni invaginaciji je bil izjemno demonstrativen. Pogostost bolečin je zelo nazorna. Na začetku izvajanja so bili premori tako dolgi, da je bolnik, ko se je umiril, očitno spal, ne da bi trpel zaradi bolečih napadov.
Bolečina pri invaginacijah prebavil očitno ni značilna v smislu lokalizacije kot pri vseh. boli želodec, pri ileocekalnih izvedbah pa se bolečina sprva čuti na desni v predelu ilea, nato pa se razširi že na ves želodec.
Bolečine pri invaginacijah so lahko odvisne od dveh razlogov:v - prvem, od dejstva, da pri pri izvajanju je črevesna mezenterija omejena in stena črevesja, v kateri se intususceptum premika naprej, se nerazumno raztegne; drugič, zaradi konvulzivnega zmanjšanja zgornjih črevesnih oddelkov v poskusu potiskanja njihove vsebine skozi oviro. Zaradi takšnega dvojnega mehanizma bolečine pri invaginacijah so lahko svojevrstne. Tako je eden od bolnikov I. G. Rufanova na primer zagotovil, da se počuti, "kot črevo vstopi v črevo"; bolan MB Zamoshchina z invaginacijo jejunuma v želodcu (pri gastroterostomozi) je poročal, da je ob začetku bolezni čutil, "da se je v želodcu nekaj zlomilo" itd. V vsakem primeru se invaginacijske bolečine bistveno razlikujejo po značaju od bolečin pri akutnem apendicitu. , adnexites, ie from pains at purely inflammatory changes from which, apparently, in many cases they can be differentiated. Unlike the alternating pains, pains constants are sometimes observed. On Vortmanna, such constant pains are characteristic of quickly coming necrosis of the restrained intussusceptum.
Very often vomiting disturbs patients. At the beginning of a disease there can be purely reflex vomiting depending on infringement of a mesentery. Then, with advance of an intussusceptum in depth of an intestinal gleam, vomiting can renew again. In most cases the fecal vomit at invaginations happens only before a lethal outcome. Such invaginatsionny vomiting differs from kalopodobny vomiting markedly at cholelithic impassability at which this symptom happens quite frequent in initial stages.
In emetic masses there is nothing characteristic. But at enteric and gastric invaginations vomiting, on the contrary, is very characteristic because it almost always happens sharply bloody. The case history of the patient operated with Schukin can be an illustration to told.
"The patient, 38 years, 16/VII 1926 g is brought to surgical department of Staritsky hospital with complaints to cruel abdominal pains and frequent vomiting. It is sick 2 days. It is operated more than 3 flyings ago (in other hospital) concerning a duodenum ulcer; after operation felt absolutely healthy all the time; ate "what got" and worked the most hard work. The beginning of this disease dates for rise in weight after very plentiful food. Suddenly there was vomiting, at first dark green color, and then painted by blood. After drink vomiting amplified, and the number of emetic masses many times over exceeded the drunk liquid.
Under the diagnosis "impassability" 18/VII — operation (Schukin) under a chloroformic anesthesia. After opening of an abdominal cavity implementation of the taking-away loop of a small bowel throughout 8 — 10 cm in a pozadiobodochny anastomosis is revealed. The invaginated part of a gut of dark color, is edematous. It is easily extended from a stomach. From the former ulcer there is no trace left also. Deaf stitches are put. 20/VII the patient died".
In the given case history vomiting blood was once; at some patients the hematemesis repeats several times, at the same time emetic masses consists almost of pure blood. This symptom should be considered as for enteric and gastric invaginations a hematemesis very a patognomonichna.
Quite often patients complain of disturbance of the correct action of intestines. At invaginations there can be or complete cessation of an otkhozhdeniye a calla and gases, or, on the contrary, increase of a chair with an otkhozhdeniye of liquid excrements with slime and impurity of blood, or increase of a chair with liquid excrements, but without blood impurity.
Usually it is considered that at invaginations there has to be a bloody chair and if it is absent, then the diagnosis of invagination is called into question. It is incorrect. The statistics of frequency of a bloody chair at adults is heterogeneous. So, Weiss observed a bloody chair in 74%, Vortmann — in 38%, and I. G. Rufanov — only in 8 — 10%. In view of this distinction, follows, it seems to us, to reckon with this symptom when it happens, but not to wait for it emergence for confirmation of the diagnosis.
The tenesmus which are observed at invaginations are especially painful at colic invaginations and are absent at enteric.
It settles the main complaints of patients at intestinal invaginations. Other subjective symptoms — weakness, thirst, appetite loss, nausea, dryness in a mouth and so forth, are inherent in general to intestinal impassability and for intestinal implementation represent nothing specific.
Objective research. At the beginning of a disease at emergence of pains and vomitings at children shock is, as a rule, observed. At adult such general changes can not be. Pulse remains full, equal, normal or close to norm of frequency. At the very beginning of a disease pulse can be even slowed down. A little also temperature remaining subfebrile changes. In a further current pulse can become frequent considerably, reflecting weight of invagination and degree of intestinal impassability — full or relative.
Language, heart, lungs are not exposed to big changes. It is necessary to pay special attention to an abdominal cavity and to those changes in it which can be caught already in early stages of a course of a disease.
The data obtained at usual clinical inspection can be heterogeneous that depends, clear, from a variety of forms of invaginations. It is easy to imagine that during the first hours even high implementation the stomach can be and it is not blown up as the intestinal piece lying over invagination kept still the tone, • its contents, however, hardly, but after all move ahead through an intussusceptum thanks to what gas exchange and sokoobmen throughout a digestive tract are still supported. The same can occur also at low invaginations when there is no full impassability.
We will give two case histories relating to two invaginations almost at the same level, but variously proceeding in dependence, apparently, on completeness of obstruction of an intestinal gleam. The first concerns the patient whom we observed in clinic (V. I. Ivankovich).
The patient, 45 years, is brought to clinic of 25/VIII 1936 g in 6 hours from the beginning of pains in the right ileal area. Ached suddenly, among full health. Pains were followed by vomiting. Similar pains happened earlier, proceeding for 2 — 3 days. Temperature 37,4 °. Pulse 76.
Objectively. The stomach is not blown up, participates in breath. The right half of an abdominal wall is a little strained and painful at palpation. Symptoms of Rovzinga, Shchetkin — Blyumberg poorly positive. In the field of a point Mack-Byorni is defined a swelling by size about egg. The swelling is a little mobile.
At urgent operation caecum invagination with a worm-shaped shoot in the ascending gut was found. Disinvagination, appendectomy and a typhlopexy are made. The patient recovered.
In the given case history it is specified that no abdominal distention existed. The general state was satisfactory. For invagination the acute beginning, pains in an abdominal cavity and existence of a tumor in 6 hours from the beginning of a disease was pathognomonic.
Absolutely the patient described by E. V. Vasilyevsky had other current.
The patient, 39 years, came to 8 o'clock in the evening 28/V 1913 g. Complains of the strongest abdominal pains. Good addition, satisfactory food. Hardly owing to severe pains in a stomach says that ached the day before, about 7 o'clock in the evening. Earlier similar attacks happened, but not in such degree. Since remembers himself from time to time there were attacks of abdominal pains, mainly in an anticardium or near a navel which kept sometimes till 2 days. Cannot connect with something emergence of pains. In the childhood of pain were less; especially often they were during stay of the patient on military service. Attacks happened
various force. Sometimes pains did not develop long, till some months. The chair always was correct; never noticed blood in excrements. There was several times vomiting. Is not a purgative.
Objectively. Two small tumors are determined by the white line above a navel, and one about large haricot, dense, is very painful (the patient does not allow to touch it). During stay served in the forces of the patient the pains reminding present once; to it then suggested to remove a tumor, but he did not agree.
The stomach is blown strongly up, at palpation is painful and strongly strains; at percussion — everywhere the tympanic sound which is slightly dulled in sloping places. Pulse 120, weak filling. Temperature 37,5 °. At urgent operation the tumor size about a fist which was implementation of a caecum in ascending and partly in cross colonic is found "at the lower surface of a liver. Disinvagination is made. The patient recovered.
The given E. V. Vasilyevsky's supervision on invagination height very reminds V. I. Ivankovich's supervision; they differ a little on disease terms; one patient suffered 6 hours, another — 25 hours. They are not similar at each other and on local and to the general symptoms. In case of V. I. Ivankovich the patient had a stomach of a normal configuration, the abdominal wall participated in breath; at sick E. V. Vasilyevsky the stomach was blown up, intense. The first patient had a pulse 76, at the second — 120! It is possible to explain various condition of patients not only terms of supervision, but also and degree of tightness of obturation on site to invagination as it is known that full of obturation proceed hard, incomplete — it is much easier.
The intestinal peristaltics seen through belly covers is of considerable interest. This phenomenon also depends on degree of tightness of obstruction, but, besides, and on height of implementation and terms of a disease. From a case history of the patient operated with P. N. Napalkov (p. 185) with postoperative invagination it is visible how the intestinal peristaltics gradually appeared, accruing with time and with impassability degree. It is clear, that emergence of the vermicular movement of intestinal loops seen through an abdominal wall requires existence over an intussusceptum of their some piece therefore very high enteric invaginations can proceed also without visible vermicular movement.
Enormous value for recognition of implementations has detection at palpation of an abdominal cavity of the pasty, mobile education similar sometimes to a sphere, at times on the roller, sausage and so forth. This tumor can vanish during research, and at a palpation in the period of painful attacks can be reduced in sizes. At palpation of such tumors can appear calmed down again there were pains; such tumors not in all cases of intestinal invaginations are probed; according to I. G. P at f and N about in at, at enteric implementations are found in 40% of cases, at colic — in 80%, and at thinly - colic — in 65 — 70%.
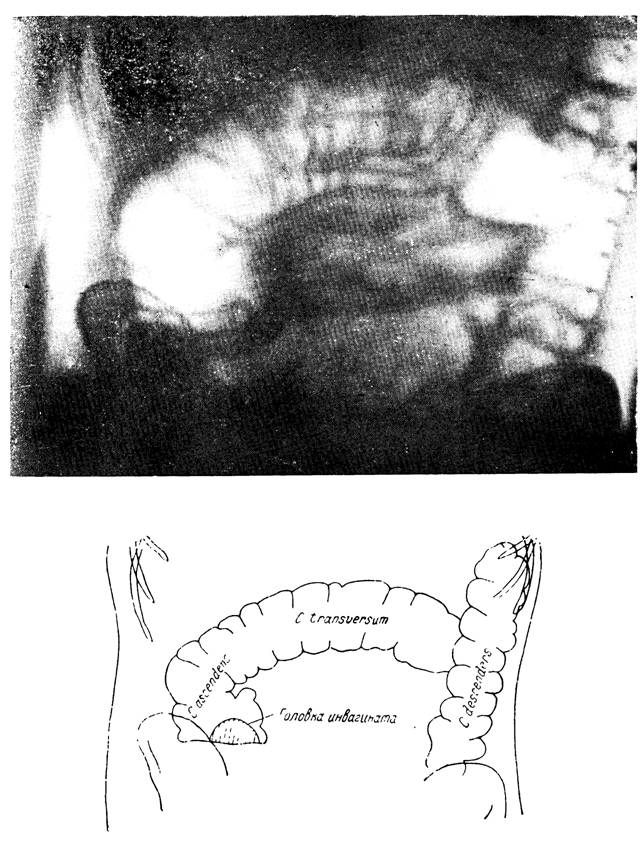
Fig. 27. A X-ray pattern at ileocecal invagination
(supervision of doctor O. O. D e N) (from a collection E. A. Pchelina).
The picture is made in vertical position of the patient. Research was made by means of inflation of air through a rectum. Against the large intestine inflated by gas with its characteristic topography and gaustralny protrusions of a wall in a gleam of a gut the horizontal level of liquid against a wing of the right ileal bone is visible. Over level the intensive shadow with a roundish contour — the intussusceptum head comprising an ileal gut acts. As a result of the applied manipulations — spontaneous disinvagination.
Feeling an abdominal cavity at invaginations, it is necessary to estimate a degree of admission of the right ileocecal area. At implementations of a small bowel in thick it is considered that the right ileal hollow becomes empty and this emptiness can be felt at a palpation. This symptom carries the name of a sign D and N with and, it is described, apparently, in all articles treating about invaginations including its pathognomonic for this disease. In my opinion, it is a little wrong. At ileocecal torsions the caecum is displaced, and on its place emptiness would have to be formed. Such point of view V. G. Ts e e - M adhered and to N of t e y f e l; he considered that emptiness in the right ileal hollow is characteristic of torsions of a gut and calls it O. G. Shiman's sign. There can be all this to some extent and fairly, but is absolutely unclear. Why at caecum shift the vacant place is not taken by other intestinal loops, and it has to remain by all means empty? This question is absolutely fairly raised by Vortmann, critically approaching Dans's sign.
When listening an abdominal cavity it is possible to catch the most various sounds (rumbling, gurgle, transfusion etc.), but in them there is nothing specific to invagination as they can meet at any relative impassability. Quite often determine by percussion existence in a free abdominal cavity of the moving liquid.
Finish clinical trial of the patient with obligatory survey of an anus with introduction of a finger to a rectum. Survey of an anus can give a valuable sign, find its gaping. The gaping appears because an intussusceptum, having reached an anus, mechanically slightly stretches it. When slipping an intussusceptum out of limits of an anal press diagnosis becomes simpler as the intussusceptum lies directly before eyes of investigating. However, despite, apparently, simplicity of diagnosis in similar cases, mistakes after all can be:the intussusceptum which sliped through an anal press is taken for the dropped-out rectum. In these cases the issue is resolved by manual research:at a prolapse of the rectum it is possible to enter a finger only into the center of the dropped-out tube, at loss of an intussusceptum it is possible to bypass it a finger but circles and, besides, to enter a finger into the center of an intussusceptum.
By means of manual research it is also possible to find the intussusceptum which stopped somewhere in a rectum and traces of the blood which is absent in excrements.
 Nanotehnologija in diagnoza in zdravljenje COVID-19
Nanotehnologija in diagnoza in zdravljenje COVID-19
 10 preprostih nasvetov SIBO za okrevanje po božičnem pretiravanju
10 preprostih nasvetov SIBO za okrevanje po božičnem pretiravanju
 Prebavne motnje:presenetljivi razlogi, zakaj imate pline
Prebavne motnje:presenetljivi razlogi, zakaj imate pline
 Kako kakovost zraka in pitna voda vplivata na zdravje črevesja
Kako kakovost zraka in pitna voda vplivata na zdravje črevesja
 Svetovni dan zdravja – pogovorimo se o SIBO
Svetovni dan zdravja – pogovorimo se o SIBO
 Povezava med astmo in refluksom kisline
Povezava med astmo in refluksom kisline
 Ali je streptokokno grlo nalezljivo? 12 simptomov in znakov
Kaj je strep grlo? Če se strepno grlo zdravi z antibiotiki, po 24 urah ni več nalezljivo. Strep grlo je nalezljiva okužba grla, ki jo običajno povzroča streptokok skupine A bakterije. Inkubacijska d
Ali je streptokokno grlo nalezljivo? 12 simptomov in znakov
Kaj je strep grlo? Če se strepno grlo zdravi z antibiotiki, po 24 urah ni več nalezljivo. Strep grlo je nalezljiva okužba grla, ki jo običajno povzroča streptokok skupine A bakterije. Inkubacijska d
 Žalostno stanje ameriške medicine:zakaj bolniki in zdravniki trpijo (in kako lahko to popravimo)
Napisal sem nekaj grdih, groznih in naravnost zlobnih objav na blogu ... In jih naslednji dan izbrisal. Nikoli jih ne boste prebrali. Prišli so z mesta bolečine in bolečine. Nikomur ne bodo služili
Žalostno stanje ameriške medicine:zakaj bolniki in zdravniki trpijo (in kako lahko to popravimo)
Napisal sem nekaj grdih, groznih in naravnost zlobnih objav na blogu ... In jih naslednji dan izbrisal. Nikoli jih ne boste prebrali. Prišli so z mesta bolečine in bolečine. Nikomur ne bodo služili
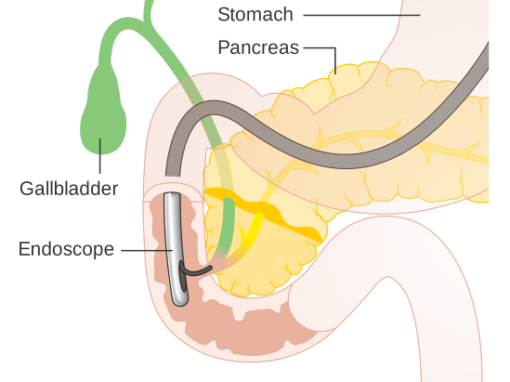 Kaj je ERCP?
Endoskopska retrogradna holangiopankreatografija ( ERCP) je endoskopski postopek, pri katerem se zgornji endoskop s stranskim pogledom usmeri v prvo palico tankega črevesa (dvanajsternika), s čimer se
Kaj je ERCP?
Endoskopska retrogradna holangiopankreatografija ( ERCP) je endoskopski postopek, pri katerem se zgornji endoskop s stranskim pogledom usmeri v prvo palico tankega črevesa (dvanajsternika), s čimer se