 Osobe s težim GERB-om mogu imati regurgitaciju hrane iz želuca u jednjak ili usta, osobito kada aktivnosti povećavaju pritisak u trbuhu, na primjer, uz kašalj i savijanje.
Osobe s težim GERB-om mogu imati regurgitaciju hrane iz želuca u jednjak ili usta, osobito kada aktivnosti povećavaju pritisak u trbuhu, na primjer, uz kašalj i savijanje.
Simptomi disfagije povezani s gutanjem
Najčešći simptom disfagije pri gutanju je osjećaj da se progutana hrana lijepi, bilo u donjem dijelu vrata ili u prsima.
S neurološkim problemima može doći do poteškoća s pokretanjem gutanja jer se hrana ne može ugurati jezikom u grlo.
Starije osobe s protezom možda neće dobro žvakati hranu i stoga gutaju velike komade čvrste hrane koji se zaglave.
Disfagija je medicinski izraz za simptom otežanog gutanja, koji potječe od latinske i grčke riječi što znači poteškoće s jelom.
Gutanje je složena radnja.
S obzirom na njegovu složenost, nije čudo da je gutanje, počevši od kontrakcije gornjeg ždrijela, "automatizirano", što znači da za gutanje nije potrebna nikakva misao nakon što se gutanje započne. Gutanje je kontrolirano automatskim refleksima koji zahvaćaju živce unutar ždrijela i jednjaka, kao i centar za gutanje u mozgu koji je živcima povezan sa ždrijelom i jednjakom. (Refleks je mehanizam koji se koristi za kontrolu mnogih organa. Refleksima su potrebni živci unutar organa kao što je jednjak da bi osjetili što se događa u tom organu i poslali informacije drugim živcima u stijenci organa ili izvan organa Informacija se obrađuje u tim drugim živcima i određuju se odgovarajući odgovori na stanja u organu. Zatim drugi živci šalju poruke iz živaca za obradu natrag u organ kako bi kontrolirali funkciju organa, na primjer, kontrakciju mišića organa. U slučaju gutanja, procesiranje refleksa prvenstveno se događa u živcima unutar stijenke ždrijela i jednjaka te u mozgu.)
Složenost gutanja također objašnjava zašto postoji toliko mnogo uzroka disfagije. Problemi se mogu pojaviti sa:
Problemi mogu biti unutar ždrijela ili jednjaka, na primjer, s fizičkim suženjem ždrijela ili jednjaka. Disfagija također može biti posljedica bolesti mišića ili živaca koji kontroliraju mišiće ždrijela i jednjaka ili oštećenja centra za gutanje u mozgu. Konačno, ždrijelo i gornja trećina jednjaka sadrže mišiće koji su isti kao mišići koje koristimo dobrovoljno (kao što su mišići ruku) koji se nazivaju skeletni mišići. Donje dvije trećine jednjaka sastoji se od različite vrste mišića poznatog kao glatki mišići. Dakle, bolesti koje zahvaćaju prvenstveno skeletne mišiće ili glatke mišiće u tijelu mogu utjecati na ždrijelo i jednjak, dodajući dodatne mogućnosti uzrocima disfagije.
Postoje dva simptoma koja se često smatraju problemima s gutanjem (disfagija), a vjerojatno nisu. Ovi simptomi su odinofagija i globusni osjećaj.
Odinofagija znači bolno gutanje. Ponekad pojedincima nije lako razlikovati odinofagiju i disfagiju. Na primjer, hrana koja se zaglavi u jednjaku često je bolna. Je li ovo disfagija ili odinofagija ili oboje? Tehnički je riječ o disfagiji, ali pojedinci je mogu opisati kao bolno gutanje (tj. odinofagija). Štoviše, pacijenti s gastroezofagealnom refluksnom bolešću (GERB) mogu opisati disfagiju kada je ono što stvarno imaju odinofagija. Bol koji osjećaju nakon gutanja nestaje kada se upala GERB-a liječi i nestaje, a vjerojatno je posljedica boli uzrokovane hranom koja prolazi kroz upaljeni dio jednjaka.
Odinofagija se također može pojaviti kod drugih stanja povezanih s upalom jednjaka, na primjer, virusne i gljivične infekcije. Važno je razlikovati disfagiju i odinofagiju jer uzroci svakog od njih mogu biti prilično različiti.
Osjećaj globusa odnosi se na osjećaj da je u grlu knedla. Kvržica može biti prisutna kontinuirano ili samo pri gutanju. Uzroci osjeta globusa su različiti, a često se ne pronađe uzrok. Osjet globusa se na različite načine pripisuje abnormalnoj funkciji živaca ili mišića ždrijela i GERB-u. Osjet globusa obično jasno opisuju pojedinci i rijetko uzrokuje zabunu s pravom disfagijom.
Kao što je već spomenuto, postoji mnogo uzroka disfagije. Radi praktičnosti, uzroci disfagije mogu se razvrstati u dvije skupine;
Uzroci se također mogu različito klasificirati u nekoliko skupina.
S neurološkim problemima može doći do poteškoća s pokretanjem gutanja jer bolus ne može biti potisnut jezikom u grlo. Starije osobe s protezom možda neće dobro žvakati hranu i stoga gutaju velike komade čvrste hrane koji se zaglave. (Unatoč tome, to se obično događa kada postoji dodatni problem unutar ždrijela ili jednjaka kao što je striktura.)
Međutim, najčešći simptom disfagije pri gutanju je osjećaj da se progutana hrana lijepi, bilo u donjem dijelu vrata ili u prsima. Ako se hrana zaglavi u grlu, može doći do kašljanja ili gušenja uz iskašljavanje progutane hrane. Ako hrana uđe u grkljan, isprovocirat će se jači kašalj i gušenje. Ako meko nepce ne radi i ne zatvara pravilno nazalne prolaze, hrana – osobito tekućina – može povratiti u nos s gutanjem. Ponekad se hrana može vratiti u usta odmah nakon gutanja.
Hrana koja se zalijepi u jednjak može tamo ostati dulje vrijeme. To može stvoriti osjećaj punjenja prsa kako se više hrane pojede i rezultirati time da pojedinac mora prestati jesti i možda piti tekućinu u pokušaju da ispere hranu. Nemogućnost jesti veće količine hrane može dovesti do gubitka težine. Osim toga, hrana koja ostaje u jednjaku može regurgitirati iz jednjaka noću dok pojedinac spava, a pojedinac se može probuditi kašljem ili gušenjem usred noći što je izazvano hranom koja regurgitira. Ako hrana uđe u grkljan, dušnik i/ili pluća, može izazvati epizode astme, pa čak i dovesti do infekcije pluća i aspiracijske upale pluća. Ponavljajuća upala pluća može dovesti do ozbiljne, trajne i progresivne ozljede pluća. Povremeno, pojedince ne probudi iz sna hrana koja povrati, već se probude ujutro kako bi na svom jastuku pronašli povratnu hranu.
Osobe koje zadržavaju hranu u jednjaku mogu se žaliti na simptome nalik žgaravici (GERB). Njihovi simptomi mogu doista biti posljedica GERB-a, ali vjerojatnije su zbog zadržane hrane i ne reagiraju dobro na liječenje GERB-a.
Kod spastičnih poremećaja motiliteta, pojedinci mogu razviti epizode boli u prsima koje mogu biti toliko jake da oponašaju srčani udar i uzrokuju odlazak u hitnu pomoć. Uzrok boli kod spastičnih poremećaja jednjaka je nejasan, iako je vodeća teorija da je posljedica spazma mišića jednjaka.
Odinofagija i globusni osjećaj. Već se raspravljalo o povremenim poteškoćama u razlikovanju disfagije od odinofagije, kao i o razlici između disfagije i globusnog osjeta.
Traheo-ezofagealna fistula. Jedan poremećaj koji se može zamijeniti s disfagijom je traheo-ezofagealna fistula. Traheo-ezofagealna fistula je otvorena komunikacija između jednjaka i dušnika koja se često razvija zbog karcinoma jednjaka, ali se također može pojaviti kao prirođena (urođena) mana. Progutana hrana može izazvati kašalj koji oponaša kašalj zbog disfunkcije mišića ždrijela koja omogućuje ulazak hrane u grkljan; međutim, u slučaju fistule, kašalj je posljedica prolaska hrane iz jednjaka kroz fistulu u dušnik.
Sindrom ruminacije. Sindrom ruminacije je sindrom u kojem se hrana bez napora vraća u usta nakon što je obrok završen. Obično se javlja kod mlađih žena i vjerojatno se može zamijeniti s disfagijom. Međutim, nakon gutanja nema osjećaja lijepljenja hrane.
Gastroezofagealna refluksna bolest (GERB). Ljudi s težim GERB-om mogu imati regurgitaciju hrane iz želuca u jednjak ili usta, osobito kada aktivnosti povećavaju pritisak u trbuhu, na primjer, uz kašalj i savijanje. Regurgitacija se također može pojaviti noću dok osobe s GERB-om spavaju, kao u onih s poremećajima gutanja kojima se hrana skuplja u jednjaku.
Srčana bolest. Poremećaji spastičnog motiliteta koji uzrokuju disfagiju mogu biti povezani sa spontanom boli u prsima, odnosno boli u prsima koja nije povezana s gutanjem. Unatoč prisutnosti disfagije, uvijek se mora pretpostaviti da je spontana bol u prsima posljedica bolesti srca sve dok se bolest srca ne isključi kao uzrok boli u prsima. Stoga je važno pažljivo testirati na srčanu bolest prije nego što uzmete u obzir jednjak kao uzrok boli u prsima kada se pacijent s disfagijom žali na epizode spontane boli u prsima.
Povijest pojedinca s disfagijom često daje važne naznake o temeljnom uzroku disfagije.
Priroda simptoma ili simptoma daje najvažnije naznake uzroka disfagije. Gutanje koje je teško započeti ili koje dovodi do nazalne regurgitacije, kašlja ili gušenja najvjerojatnije je posljedica oralnog ili faringealnog problema. Gutanje koje rezultira osjećajem da se hrana zalijepi u prsa (jednjak) najvjerojatnije je posljedica problema s jednjakom.
Disfagija koja brzo napreduje tijekom tjedana ili nekoliko mjeseci ukazuje na maligni tumor. Disfagija samo za krutu hranu sugerira fizičku opstrukciju prolaza hrane, dok je disfagija za krutu i tekuću hranu vjerojatnije biti uzrokovana bolešću glatkih mišića jednjaka. Također je vjerojatnije da će povremeni simptomi biti uzrokovani bolestima glatkih mišića nego opstrukcijom jednjaka jer je disfunkcija mišića često povremena.
Prethodno postojeće bolesti također daju tragove. Oni s bolestima skeletnih mišića (na primjer, polimiozitis), mozga (najčešće moždani udar) ili živčanog sustava imaju veću vjerojatnost da će imati disfagiju na temelju disfunkcije mišića i živaca orofaringeusa. Osobe s kolagenskim vaskularnim bolestima, na primjer, sklerodermijom, češće imaju problema s mišićima jednjaka, osobito neučinkovitom peristaltikom.
Bolesnici s GERB-om u anamnezi imaju veću vjerojatnost da će imati strikture jednjaka kao uzrok njihove disfagije, iako oko 20% pacijenata sa strikturama ima minimalne simptome GERB-a ili ih uopće nema prije početka disfagije. Vjeruje se da je refluks koji se javlja noću štetniji za jednjak. Također postoji veći rizik od raka jednjaka među osobama s dugotrajnim GERB-om.
Gubitak težine može biti znak ili teške disfagije ili malignog tumora. Češće od gubitka kilograma, ljudi opisuju promjenu u načinu prehrane – manji zalogaji, dodatno žvakanje – koja produljuje obroke tako da oni zadnji za stolom završavaju s jelom. Ovaj potonji obrazac, ako je prisutan dulje vrijeme, sugerira nemaligni, relativno stabilan ili sporo progresivan uzrok disfagije. Epizode boli u prsima koje nisu posljedica bolesti srca upućuju na mišićne bolesti jednjaka. Rođenje i boravak u Srednjoj ili Južnoj Americi povezani su s Chagasovom bolešću.
Fizikalni pregled ima ograničenu vrijednost u sugeriranju uzroka disfagije. Abnormalnosti neurološkog pregleda upućuju na neurološke ili mišićne bolesti. Promatranjem pojedinog gutanja može se utvrditi ima li poteškoća u pokretanju gutanja, što je znak neurološke bolesti. Tumori u vratu upućuju na mogućnost kompresije ždrijela. Traheja koja se ne može pomicati s jedne strane na drugu sugerira tumor niže u prsima koji je zarobio dušnik i možda jednjak. Promatranje atrofije (smanjene veličine) ili fasikulacije jezika (fino drhtanje) također ukazuje na bolesti živčanog sustava ili skeletnih mišića.
Endoskopija. Endoskopija uključuje umetanje dugačke (jedan metar) fleksibilne cijevi sa svjetlom i kamerom na kraju kroz usta, ždrijelo, jednjak i u želudac. Sluznica ždrijela i jednjaka može se vizualno procijeniti, a biopsije (mali komadići tkiva) mogu se dobiti za pregled pod mikroskopom ili za bakterijske ili virusne kulture.
Endoskopija je izvrstan način dijagnosticiranja tumora, striktura i Schatzkijevih prstenova, kao i infekcija jednjaka. Također je vrlo dobar za dijagnosticiranje divertikula srednjeg i donjeg jednjaka, ali loš za dijagnosticiranje divertikula u gornjem dijelu jednjaka (Zenkerov divertikulum).
Moguće je uočiti abnormalnosti mišićne kontrakcije jednjaka, ali manometrija jednjaka je test koji je mnogo prikladniji za procjenu funkcije mišića jednjaka. Resistance passing the endoscope through the lower esophageal sphincter combined with a lack of esophageal contractions is a fairly reliable sign of achalasia or Chagas disease (due to the inability of the lower esophageal sphincter to relax), but it is important when there is resistance to exclude the presence of a stricture or cancer which also can cause resistance. Finally, there is a characteristic appearance of the esophageal lining when infiltrated with eosinophils that strongly suggests the presence of eosinophilic esophagitis.
X-rays. There are two different types of X-rays that can be done to diagnose the cause of dysphagia. The barium swallow or esophagram is the simplest type. For the barium swallow, mouthfuls of barium are swallowed, and X-ray films are taken of the esophagus at several points in time while the bolus of barium traverses the esophagus. The barium swallow is excellent for diagnosing moderate-to-severe external compression, tumors, and strictures of the esophagus. Occasionally, however, Schatzki's rings can be missed.
Another type of X-ray study that can be done to evaluate swallowing is the video esophagram or video swallow, sometimes called a video-fluoroscopic swallowing study. For the video swallow, instead of several static X-ray images of the bolus traversing the esophagus, a video X-ray is taken. The video study can be reviewed frame by frame and is able to show much more than the barium swallow. This usually is not important for diagnosing tumors or strictures, which are well seen on barium swallow, but it is more effective for suggesting problems with the contraction of the muscles of the esophagus and pharynx (though esophageal manometry, discussed later, is still better for studying contraction), milder external compression of the esophagus, and Schatzki's rings. The video study can be extended to include the pharynx where it is the best method for demonstrating osteophytes, cricopharyngeal bars, and Zenker's diverticuli. A modified barium swallow is a version of the test evaluating the oropharyngeal phases of swallowing. A speech pathologist is usually involved with the evaluation to determine subtle sequence and phase abnormalities.
The video swallow also is excellent for diagnosing penetration of barium (the equivalent of food) into the larynx and trachea due to neurological and muscular problems of the pharynx that may be causing coughing or choking after swallowing food.
Esophageal manometry. Esophageal manometry, also known as esophageal motility testing, is a means to evaluate the function of pharyngeal and esophageal muscles. For manometry, a thin, flexible catheter is passed through the nose and pharynx and into the esophagus. The catheter is able to sense pressure at multiple locations along its length in both the pharynx and the esophagus. When the pharyngeal and esophageal muscles contract, they generate a pressure on the catheter which is sensed, measured and recorded from each location. The magnitude of the pressure at each pressure-sensing location and the timing of the increases in pressure at each location in relation to other locations give an accurate picture of how the muscles of the pharynx and esophagus are contracting.
The value of manometry is in diagnosing and differentiating among diseases of the muscle or the nerves controlling the muscles that result in muscle dysfunction of the pharynx and esophagus. Thus, it is useful for diagnosing the swallowing dysfunction caused by diseases of the brain, skeletal muscle of the pharynx, and smooth muscle of the esophagus.
Esophageal impedence. Esophageal impedence testing utilizes catheters similar to those used for esophageal manometry. Impedence testing, however, senses the flow of the bolus through the esophagus. Thus, it is possible to determine how well the bolus is traversing the esophagus and correlate the movement with concomitantly recorded esophageal pressures determined by manometry. (It also can be used to sense reflux of stomach contents into the esophagus among patients with GERD.) Multiple sites along the length of the esophagus can be tested to assess the movement of the bolus and presence of reflux, including how high up it extends.
Esophageal acid testing. Esophageal acid testing is not a test that directly diagnoses diseases of the esophagus. Rather, it is a method for determining whether or not there is reflux of acid from the stomach into the esophagus, a cause of the most common esophageal problem leading to dysphagia, esophageal stricture. For acid testing, a thin catheter is inserted through the nose, down the throat, and into the esophagus. At the tip of the catheter and placed just above the junction of the esophagus with the stomach is an acid-sensing probe. The catheter coming out of the nose passes back over the ear and down to the waist where it is attached to a recorder. Each time acid refluxes (regurgitates) from the stomach and into the esophagus it hits the probe, and the reflux of acid is recorded by the recorder. At the end of a prolonged period, usually 24 hours, the catheter is removed and the information from the recorder is downloaded into a computer for analysis. Most people have a small amount of reflux of acid, but individuals with GERD have more. Thus, acid testing can determine if GERD is likely to be the cause of the esophageal problem such as a stricture, as well as if treatment of GERD is adequate by showing the amount of acid that refluxes during treatment is normal.
An alternative method of esophageal acid testing uses a small capsule containing an acid-sensing probe that is attached to the esophageal lining just above the junction of the esophagus with the stomach. The capsule wirelessly transmits the presence of episodes of acid regurgitation to a receiver carried on the chest. The capsule records for two or three days and later is shed into the esophagus and passes out of the body in the stool.
Other tests The diagnosis of muscular dystrophies and metabolic myopathies usually involves a combination of tests including blood tests that can suggest muscle injury, electromyograms to determine if nerves and muscles are working normally, biopsies of muscles, and genetic testing.
The treatment of dysphagia varies and depends on the cause of the dysphagia. One option for supporting patients either transiently or long-term until the cause of the dysphagia resolves is a feeding tube. The tube for feeding may be passed nasally into the stomach or through the abdominal wall into the stomach or small intestine. Once oral feeding resumes, the tube can be removed.
Treatment for obstruction of the pharynx or esophagus requires removal of the obstruction.
Tumors usually are removed surgically although occasionally they can be removed endoscopically, totally or partially. Radiation therapy and chemotherapy also may be used particularly for malignant tumors of the pharynx and its surrounding tissues. If malignant tumors of the esophagus cannot be easily removed or the tumor has spread and survival will be limited, swallowing can be improved by placing stents within the esophagus across the area of obstruction. Occasionally, obstructing tumors can be dilated the same way as strictures. (See below.)
Strictures and Schatzki's rings usually are treated with endoscopic dilation, a procedure in which the narrowed area is stretched either by a long, semi-rigid tube passed through the mouth or a balloon that is blown up inside the esophagus.
The most common infiltrating disease causing dysphagia is eosinophilic esophagitis which usually is successfully treated with swallowed corticosteroids. The role of food allergy as a cause of eosinophilic esophagitis is debated; however, there are reports of using elimination diets to identify specific foods that are associated with allergy. Elimination of these foods has been reported to prevent or reverse the infiltration of the esophagus with eosinophils, particularly in children.
Diverticuli of the pharynx and esophagus usually are treated surgically by excising them. Occasionally they can be treated endoscopically. Cricopharyngeal bars are treated surgically by cutting the thickened muscle. Osteophytes also can be removed surgically.
Congenital abnormalities of the esophagus usually are treated surgically soon after birth so that oral feeding can resume.
As previously discussed, strokes are the most common disease of the brain to cause dysphagia. Dysphagia usually is at its worst immediately after the stroke, and often the dysphagia improves with time and even may disappear. If it does not disappear, swallowing is evaluated, usually with a video swallowing study. The exact abnormality of function can be defined and different maneuvers can be performed to see if they can counter the effects of the dysfunction. For example, in some patients it is possible to prevent aspiration of food by turning the head to the side when swallowing or by drinking thickened liquids (since thin liquids is the food most likely to be aspirated).
Tumors of the brain, in some cases, can be removed surgically; however, it is unlikely that surgery will reverse the dysphagia. Parkinson's disease and multiple sclerosis can be treated with drugs and may be useful in patients with dysphagia.
Achalasia is treated like a stricture of the esophagus with dilation, usually with a balloon. A second option is surgical treatment in which the muscle of the lower esophageal sphincter is cut (a myotomy) in order to reduce the pressure and obstruction caused by the non-relaxing sphincter. Drugs that relax the sphincter usually have little or a transient effect and are useful only when achalasia is mild.
An option for individuals who are at high risk for surgery or balloon dilation is injection of botulinin toxin into the sphincter. The toxin paralyzes the muscle of the sphincter and causes the pressure within the sphincter to decrease. The effects of botulinin toxin are transient, however, and repeated injections usually are necessary. It is best to treat achalasia early before the obstruction causes the esophagus to enlarge (dilate) which can lead to additional problems such as food collecting above the sphincter with regurgitation and aspiration.
In other spastic motility disorders, several drugs may be tried, including anti-cholinergic medications, peppermint, nitroglycerin, and calcium channel blockers, but the effectiveness of these drugs is not clear and studies with them are nonexistent or limited.
For patients with severe and uncontrollable symptoms of pain and/or dysphagia, a surgical procedure called a long myotomy occasionally is performed. A long myotomy is similar to the surgical treatment for achalasia but the cut in the muscle is extended up along the body of the esophagus for a variable distance in an attempt to reduce pressures and obstruction to the bolus.
There is no treatment for ineffective peristalsis, and individuals must change their eating habits. Fortunately, ineffective peristalsis infrequently causes severe dysphagia by itself. When moderate or severe dysphagia is associated with ineffective peristalsis it is important to be certain that there is no additional obstruction of the esophagus, for example, by a stricture due to GERD, that is adding to the effects of reduced muscle function and making dysphagia worse than the ineffective peristalsis alone. Most causes of obstruction can be treated.
There are effective drug therapies for polymyositis and myasthenia gravis that should also improve associated dysphagia. Treatment of the muscular dystrophies is primarily directed at preventing deformities of the joints that commonly occur and lead to immobility, but there are no therapies that affect the dysphagia. Corticosteroids and drugs that suppress immunity sometimes are used to treat some of the muscular dystrophies, but their effectiveness has not been demonstrated.
There is no treatment for the metabolic myopathies other than changes in lifestyle and diet.
Diseases that reduce the production of saliva can be treated with artificial saliva or over-the-counter and prescription drugs that stimulate the production of saliva.
There is no treatment for Alzheimer's disease.
With the exception of dysphagia caused by stroke for which there can be marked improvement, dysphagia from other causes is stable or progressive, and the prognosis depends on the underlying cause, its tendency to progress, the availability of therapy, and the response to therapy.
Recent developments in the diagnostic arena are beginning to bring new insights into esophageal function, specifically, high resolution and 3D manometry, and endoscopic ultrasound.
High resolution and 3D manometry
High resolution and 3D manometry are extensions of standard manometry that utilize similar catheters. The difference is that the pressure-sensing locations on the catheters are very close together and ring the catheter. Recording of pressures from so many locations gives an extremely detailed picture of how esophageal muscle is contracting. The primary value of these diagnostic procedures is that they "integrate" the activities of the esophagus so that the overall pattern of swallowing can be recognized, which is particularly important in complex motility disorders. In addition, their added detail allows the recognition of subtle abnormalities and hopefully will be able to help define the clinical importance of subtle abnormalities of muscle contraction associated with lesser degrees of dysphagia.
Endoscopic ultrasonography has been available for many years but has recently been applied to the evaluation of esophageal muscle diseases. Ultrasound uses sound waves to penetrate tissues. The sound waves are reflected by the tissues and structures they encounter, and, when analyzed, the reflections give information about the tissues and structures from which they are reflected. In the esophagus, endoscopic ultrasonography has been used to determine the extent of penetration of tumors into the esophageal wall and the presence of metastases to adjacent lymph nodes. More recently, endoscopic ultrasonography has been used to obtain a detailed look at the muscles of the esophagus. What has been found is that in some disorders, particularly the spastic motility disorders, the muscle of the esophagus is thickened. Moreover, thickening of the muscle sometimes can be recognized only by ultrasonography even when spastic abnormalities are not seen with manometry. The exact role of endoscopic ultrasonography has not yet been determined but is an exciting area for future research.
 Što me dr. Tom O'Bryan naučio o poremećajima povezanim s glutenom
Što me dr. Tom O'Bryan naučio o poremećajima povezanim s glutenom
 Kako neki virusi uzrokuju rak
Kako neki virusi uzrokuju rak
 Vrijeme kada sam otpustio svog liječnika (i važne promjene privatnog savjetovanja)
Vrijeme kada sam otpustio svog liječnika (i važne promjene privatnog savjetovanja)
 Korištenje FLUOstar Omega za proučavanje novih crijevnih bakterija koje mogu utjecati na naše zdravlje
Korištenje FLUOstar Omega za proučavanje novih crijevnih bakterija koje mogu utjecati na naše zdravlje
 Inflamatorna bolest zdjelice (PID)
Inflamatorna bolest zdjelice (PID)
 Kako se testirati na SIBO
Kako se testirati na SIBO
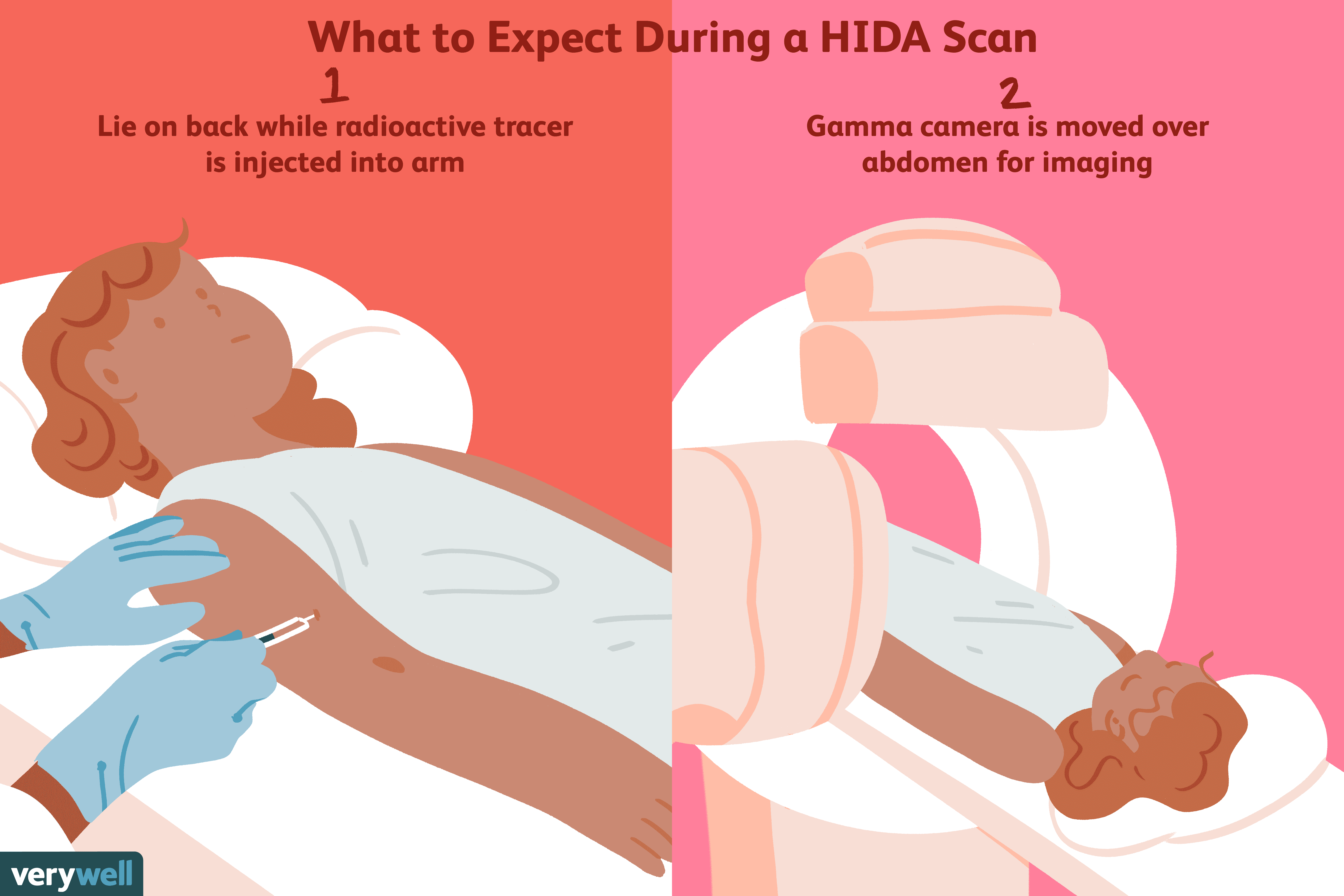 Što je skeniranje hepatobilijarne iminodijaoctene kiseline (HIDA)?
Skeniranje hepatobilijarne iminodiacetnom kiselinom (HIDA), koje se ponekad naziva i kolescintigrafija ili hepatobilijarna scintigrafija, vrsta je nuklearnog slikovnog testa koji se radi za pregled žu
Što je skeniranje hepatobilijarne iminodijaoctene kiseline (HIDA)?
Skeniranje hepatobilijarne iminodiacetnom kiselinom (HIDA), koje se ponekad naziva i kolescintigrafija ili hepatobilijarna scintigrafija, vrsta je nuklearnog slikovnog testa koji se radi za pregled žu
 Perkutana endoskopska gastrostomija (PEG)
Centar za perkutanu endoskopsku gastrostomiju (PEG) Ispunite kviz o pankreatitisu Pojačajte zdravlje probave Digestivne distrese:problematična hrana koju treba izbjegavati Činjenice o perkutanoj end
Perkutana endoskopska gastrostomija (PEG)
Centar za perkutanu endoskopsku gastrostomiju (PEG) Ispunite kviz o pankreatitisu Pojačajte zdravlje probave Digestivne distrese:problematična hrana koju treba izbjegavati Činjenice o perkutanoj end
 Evo kako crijeva i probava utječu na vaš san
Otkrijte kako crijeva i san međusobno djeluju kako bi utjecali na probavu, metabolizam, pa čak i mentalno zdravlje, te kako iskoristiti moć sna za poboljšanje dobrobiti.. Postoji mnogo razloga zašto
Evo kako crijeva i probava utječu na vaš san
Otkrijte kako crijeva i san međusobno djeluju kako bi utjecali na probavu, metabolizam, pa čak i mentalno zdravlje, te kako iskoristiti moć sna za poboljšanje dobrobiti.. Postoji mnogo razloga zašto