Cøliaki har mange uudtalte forfærdelige sandheder...
En af dem er denne:Det tager i gennemsnit 4 år at få en Cøliaki-diagnose, og forskningen viser ofte, at over 2 år senere er de fleste patienter stadig ikke helbredt og lider typisk, selvom de spiser strengt glutenfrit. kost. Denne artikel er et forsøg på at ændre det, for at give dig din kraft tilbage og faktisk hjælpe dig tilbage til et sundt liv.
Denne guide er skrevet til dig, den diagnosticerede cøliaki, for at forklare, hvad der sker i din krop, hvad det betyder for din fremtid, og hvordan du kan helbrede fra denne sygdom.
Det er beregnet til at udfylde de huller, din læge sandsynligvis ikke har fortalt dig (og pas på... der er så mange, at det næsten er kriminelt).
Jeg skrev dette, fordi Jordan Reasoner, min bedste ven, skulle kæmpe i 3 år for at få en diagnose, og bagefter modtog han kun en lille pakke, der fortalte ham, at han skulle spise en glutenfri diæt, og han ville være okay.
Men han var ikke...
To år efter at have fulgt den glutenfri diæt med kult-lignende strenghed... var han endnu tættere på at dø. Det virkede ikke, og lægerne slog hænderne op og sagde:
"Du snyder åbenbart diæten, og vi kan ikke hjælpe dig mere."
Desværre er dette nu normen i vores nuværende medicinske system – underuddannede og under-ressourcefulde læger, der bebrejder og misinformerer patienter om, hvad der faktisk skal til for at helbrede fra cøliaki, og hvad risikoen ved denne sygdom betyder for dit liv.
Men det behøver ikke at være sådan.
Jordan er helbredt og glad nu, og vi har siden hjulpet tusindvis af andre cøliaki-ofre, der har været igennem den samme kamp – og hjulpet dem med at få deres helbred tilbage ligesom ham.
Men jeg er stadig sur, så jeg skriver dette...
Mit mål er at hjælpe dig med at undgå vedvarende smerter – at forstå dine sundhedsrisici – og at lære, hvordan du vender tilbage til et normalt sundt liv, hvis du vælger det.
Spoiler Alert! En anden forfærdelig sandhed, de fleste mennesker med cøliaki opdager for sent:den glutenfri diæt i sig selv er ikke nok til at helbrede - mere detaljeret om dette senere.
Denne guide er altomfattende, hvilket betyder, at det vil tage dig omkring 15 minutter at læse. Og da jeg ikke ved, hvor uddannet du er, har vi sammensat en indholdsfortegnelse, så du kan springe til de vigtigste dele for dig:
Hvad er cøliaki?
Tegn, symptomer og forekomst
De farlige risici ved ubehandlet cøliaki
Cøliaki vs. glutenintolerance
Fra glutenfølsom til fuldblæst cøliaki
Forenkling af toksiciteten af gluten
Test for cøliaki og glutenintolerance
4 tests for cøliaki og glutenintolerance
Konventionel cøliaki behandling
3 Episke fejl ved konventionel behandling
Hvordan autoimmun sygdom udvikler sig
4 trin til heling af rodårsager
Konklusion
Jeg håber, du vil efterlade en kommentar eller dele dette med andre - det er vores håb, at vi kan redde manges liv med denne artikel.

Cøliaki er en autoimmun sygdom, der forårsager skade på tyndtarmen, hvilket fører til systemisk inflammation, næringsstofmalabsorption og mange andre væsentlige sundhedsproblemer. En autoimmun tilstand er en tilstand, hvor dit immunsystem bliver forvirret, og i stedet for at bekæmpe fremmede angribere, begynder det at angribe dig.
Den del af tyndtarmen, der bliver mest beskadiget, er normalt villi. Disse er små shag tæppe-lignende fremspring inde i tyndtarmen og er afgørende for vores helbred. De øger tyndtarmens overflade, afgiver fordøjelsesenzymer og hjælper med at indsamle og absorbere næringsstoffer.
Under udviklingen af cøliaki går villi fra vitale tråde til at blive fladtrykte og knækkede. Dette er dårlige nyheder for vores helbred.
Da det er en autoimmun sygdom, betyder det, at der er en trigger eller miljømæssig årsag, der skaber betændelse, immunforstyrrelser og efterfølgende problemer.
Den miljømæssige udløser for cøliaki menes kun at være gluten, og derfor er der så meget fokus på glutenfri fødevarer. Men desværre skader dette fokus på kun gluten de fleste cøliakere og dræber efter min mening faktisk nogle af dem. Mere om dette senere.
En anden forfærdelig sandhed om cøliaki er, at selvom skaden sker i tarmen, rapporterer kun 40 % af børn og 60 % af voksne fordøjelsesrelaterede symptomer.
Dette er en af de mere frustrerende dele af cøliaki - det kan forårsage problemer over hele vores krop. Dette menes at være en af grundene til, at langt de fleste cøliakipatienter (83 % – 97 %) forbliver udiagnosticerede.
De fleste mennesker har flere problemer fra listen nedenfor – hvor mange har du?
Almindelige tegn og symptomer på cøliaki:
Det, der virkelig er trist ved denne liste, er antallet af mennesker, der lider. En forskningsundersøgelse fra 2012 anslår, at omkring 0,71 % af amerikanerne har cøliaki (3 millioner i alt), hvilket betyder, at hvis du eller nogen i din familie ikke har cøliaki, har nogen, du kender, det.
De fleste eksperter mener nu, at tallet er tættere på 1 %, hvilket er nogenlunde den samme udbredelse, som findes i hele verden, inklusive Europa og Italien.
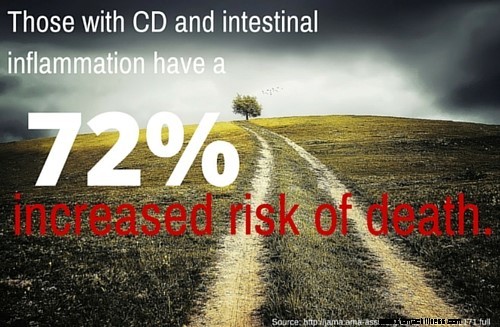
Risikoen ved at have cøliaki stopper ikke kun med symptomlisten ovenfor. Husk, at en stor procentdel (op til 60%) ikke opfatter, at de er syge, hvilket er skræmmende, når du ser på, hvordan cøliaki sætter dig op til mange andre sundhedsproblemer.
Ofte er der nogle store benægtelser, når man bliver diagnosticeret med en alvorlig sygdom som cøliaki. Og det er helt normalt, men jeg vil gerne opfordre dig til ikke at vente for længe med at tage seriøse handlinger mod helbredelse.
For hvis du ignorerer, benægter eller undlader at kontrollere dit helbredende fremskridt, vil du højst sandsynligt ende blandt en (eller mange) af disse skræmmende statistikker:
Med andre ord, hvis du er en symptomfri cøliaki, og dine laboratorier viser tegn på tarmbetændelse ... er du stadig i betydelig risiko for helbredskomplikationer og tidlig død.
Se, jeg prøver ikke at skræmme dig, jeg vil bare have, at du er en fuldt informeret patient – den slags patient, der kan træffe de bedste valg for deres krop og liv, ikke en hvis magt er i hænderne på en læge (som ærlig talt ikke har tid og opmærksomhed til at have den slags magt til at begynde med).
Og det hele starter med at se livets (til tider brutale) realiteter i øjnene.
Men bare rolig ... ovenstående scenarier behøver ikke at blive din virkelighed ... Faktisk giver jeg dig trinene til at undgå at deltage i disse statistikker (som DE fleste cøliakere), og i stedet helbrede ordentligt.
Det er ikke sådan, at du lige vågnede en dag og pludselig "fangede" Cøliaki. I stedet er du gradvist blevet mere syg, og mængden af skader inde i din krop er langsomt blevet opbygget...
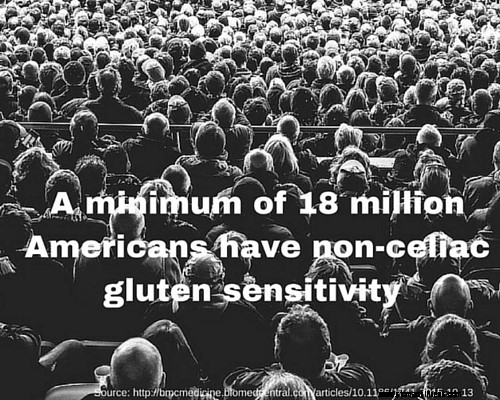
Hvilket er kerneforskellen mellem dig og dem, der lider af glutenintolerance, eller det, der også kaldes Non-Celiac Gluten Sensitivity (NCGS). University of Maryland rapporterer i øjeblikket, at omkring 18 millioner amerikanere (6 % af den amerikanske befolkning) har denne tilstand.
Dette er dog det laveste skøn over berørte mennesker...
Dr. Alessio Fasano, direktør for Center of Celiac Research, har gentagne gange sagt,
"Alle mennesker mangler de enzymer, der kræves for at nedbryde gluten."
Og nu kommer der nye undersøgelser, der foreslår mekanismer til at understøtte denne erklæring, hvilket betyder, at det faktiske antal mennesker med gluten-relaterede problemer kan være langt op i 100'erne af millioner. Det er værd at bemærke, at bare fordi det er ekstremt svært at fordøje, betyder det ikke, at alle har et glutenproblem.
Dem med glutenintolerance kan opleve alle de samme symptomer, der er anført ovenfor for cøliakere, såsom diarré eller forstoppelse, nældefeber, hjernetåge, oppustethed og hovedpine.
Ligesom cøliaki er glutenfølsomhed en tilstand, hvor immunsystemet aktiveres af gluten, hvilket forårsager betændelse og tarmpermeabilitet. Men immunsystemet angriber ikke slimhinden i tyndtarmen, som det er ved cøliaki.
Så den største forskel mellem glutenintolerance og cøliaki er den måde, immunsystemet reagerer på gluten og gliadin. Men lad os være klare, i begge tilfælde er der et immunrespons på hvede.
En NCGS-persons immunrespons er ikke rettet mod det menneskelige væv... det er rettet mod den miljømæssige trigger.
Men førende Cøliaki-eksperter, som Dr. Tom O'Bryan, mener, at Cøliaki ikke er som en lyskontakt... den tænder eller slukker ikke bare. De mener, at selv dem med NCGS har nogle immunceller, der angriber det menneskelige væv, men på et for lavt niveau til, at vores nuværende medicinske test kan opdage.
Og efter måneder eller år med dette "tavse" angreb, begynder immunresponset at vokse i sværhedsgrad, indtil det endelig kan påvises af vores nuværende laboratorietests.
Når det er sagt, hvis du er glutenintolerant, er rådene i denne artikel lige så relevante for dig som for en diagnosticeret cøliaki.
Mange cøliakere bliver faktisk ikke diagnosticeret med fuld-blæst cøliaki før senere i deres liv (20'erne, 30'erne, 40'erne, 50'erne og derover) ... hvilket er fascinerende og normalt forvirrende, når det hele sker. På dette tidspunkt spekulerer de måske på, om de var glutenintolerante hele tiden?
Lad os undersøge, hvordan cøliaki udvikler sig, og hvilken rolle glutenintolerance spiller i det - som vi husker, er forskellen mellem de to hovedsageligt i, hvor dysreguleret immunsystemet er.
Der er to hovedsider af immunsystemet - den medfødte og den adaptive. Hver spiller en stor rolle i at holde os sunde.
Ved glutenfølsomhed menes begge at aktivt angribe gluten og andre molekyler, der kommer ind i din blodbane på grund af en utæt tarm (mere om, hvad det er senere).
Ved cøliaki går den adaptive side i stykker og begynder at angribe dine tarmceller og tænker, at de også er fremmede molekyler, der bør ødelægges. Dette er den autoimmune komponent af sygdommen.
Ved både glutenfølsomhed og cøliaki er skaden og ubehaget drevet af gluten, og det er afgørende for helbredelse at undgå det. Men det er svært at undgå noget, du ikke forstår. Vi skal vide hvad præcis er gluten og hvordan vi kan undgå det.
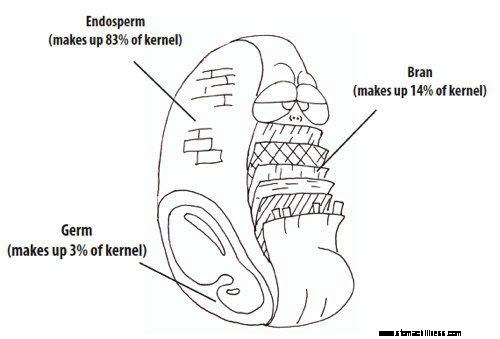
Det ved du sikkert allerede, men gluten er et protein, der findes i byg, rug og hvede.
Her er, hvad du sandsynligvis ikke ved :planter ønsker ikke at blive spist af dig. Faktisk har de en kompleks række af forsvarsmekanismer til at forhindre mennesker og andre dyr i at spise dem.
En af disse forsvarsmekanismer er giftige proteiner, kaldet prolaminer, indeholdt i stort set alle korn (glutenfri eller ej). Og gluten rummer tilfældigvis en af de mest giftige prolaminer – gliadin – og det er denne gliadin i gluten, der forårsager skaden.
Gliadin opflammer endda tarmen hos raske individer. Men for dem med glutenfølsomhed eller en genetisk disposition for cøliaki, er skaden langt værre.
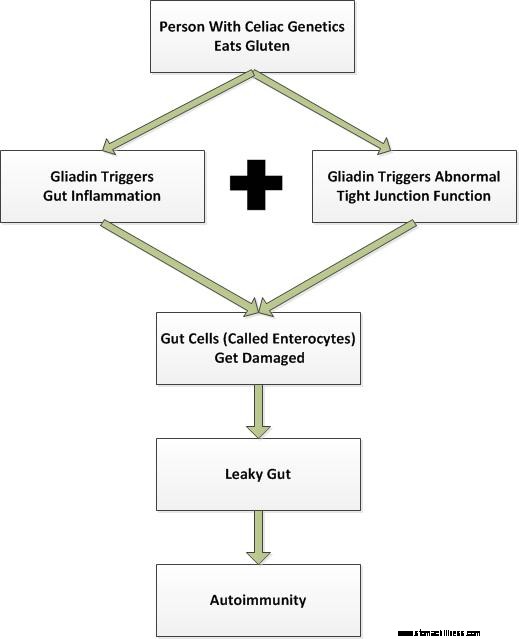
Når en person med genetik for cøliaki spiser en bagel, en skål pasta eller noget andet, der indeholder gluten, sker der skade på nogle få måder:
Stigningen i zonulin (og deraf følgende udvidelse af de tætte junctions) fører til udviklingen af en utæt tarm.
Det er værd at bemærke, at der faktisk er mindst 19 udløsere af utæt tarm - gluten er kun en af dem.
Gratis Leaky Gut-præsentation: Klik her for at lære de 19 almindelige udløsere af utæt tarm, og hvordan man helbreder fra dem.
Så kort fortalt er prolaminer forsvarsproteiner, der findes i planter. Gluten er blot en af flere typer prolaminer og indeholder en specifikt giftig del kaldet gliadin. Generelt, mens hvede, rug og byg menes at være de værste krænkere for cøliakere, kan enhver prolamin, uanset om den er fra korn eller pseudograin, være problematisk, når først skaden er begyndt.
Med det sagt, lad os tale om, hvordan man faktisk bekræfter, at du har cøliaki.
Der er meget forvirring omkring testning og diagnosticering af cøliaki og for en god ordens skyld, hvorfor det i gennemsnit tager en cøliaki 4 år at få den rigtige diagnose. Helt ærligt, det er patetisk og direkte trist. Jeg tror på, at patienter kan fremskynde denne proces ved at være mere uddannede end deres læger om emnet.
Teknisk set bestemmes en Cøliaki-diagnose baseret på histologisk demonstration med understøttende kriterier, hvilket betyder, at der ikke er én "perfekt" test til at diagnosticere sygdommen.
Det, der foregår, er, at læger leder efter en bestemt mængde skade på din tyndtarm og understøtter det med testresultater for at bekræfte, at du har risikofaktorerne for sygdommen.
In more simple terms, that means when gluten intolerance crosses a small-intestine-damage threshold and autoimmune risk factors are confirmed via lab tests or autoimmune markers are actually observed on your lab work… then you officially have the diagnosis of Celiac disease.
Since there’s so much confusion around the testing here…
Let’s break the tests into 3 categories:
1.) Supportive Tests – Typically, these are tests that that are the easiest and cheapest to run. They provide supporting evidence for risk of Celiac disease or Gluten sensitivity.
An example of a supportive test, would be getting a genetic test to check for Celiac disease genes. You can do a serum lab test or even 23andme.com testing to figure this out (meaning you don’t need to wait for your doctor to do this testing).
2.) Autoimmune Tests – These are tests used to check for and measure the level of immune system dysregulation going on in your body. There is a major drawback with these tests, though, you’ll need to have eaten gluten in the last 2-3 months to get an accurate result.
A blood test called a tTg-IgA test (Tissue Transglutaminase Test), which looks for antibodies in your blood towards gluten, is the oldest and cheapest test. However, this means there are some big drawbacks to it, including possibilities of false negatives and a positive result might mean you have something other than Celiac disease!
Bottom line for the tTg-IgA test: If you are positive or negative, it doesn’t mean you DO or DON’T have Celiac disease.
The most advanced blood test on the market, Cyrex Array 3, is the first one to check your immune reactivity to all parts of gluten, gliadin and other parts transglutaminase. This test, while still pretty new to the market, is the first of its kind to take a holistic approach in checking for wheat sensitivity. It’s currently the best option of the autoimmune tests.
3.) Damage Tests – These tests are the last step – they’re the most expensive and intrusive. However, at this time, in order to get an “official” Celiac diagnosis from a doctor, this test is the last piece of the puzzle.
It’s called an endoscopic biopsy (small intestine biopsy), and it’s where doctors actually go in and remove a part of your intestine and look at it under the microscope to check the damage. Hopefully, in the future, new testing will be developed that won’t be so invasive to the body.
In conclusion, the best approach for obtaining a proper diagnosis is to first get your genetics checked. Then, get a Cyrex Array 3. And if both are positive, get an endoscopic biopsy. If you get a positive test result from the endoscopy, it’s a big red flag you’ve had this condition for a long time and you’re likely going to need to take your healing process very seriously.
Feeling better after gluten removal isn’t enough to be diagnosed as Celiac, but it’s a really good sign that you’re AT LEAST gluten intolerant. And based on the several Cyrex Array 3 tests I’ve seen, you’d turn up plenty of positives there.
After you finally get your diagnosis, which will typically take you 4 years or longer, your conventional medical doctor will probably tell you this…
“Adopting a strict gluten-free diet is the only known treatment for those with gluten-related disorders.” – From the Celiac Disease Foundation
At first, just making this change seems so hard and sometimes impossible, especially giving up those treasured foods you may have grown up with. But the majority of Celiacs I’ve talked to finally make the change and begin to live the gluten-free lifestyle.
And they end up loving this new lifestyle because they feel so much better than before.
But most end up hitting a glass ceiling of healing. In other words, their really painful symptoms might decrease or mostly go away but they don’t get the energy, skin, hair, weight regulation and dependable brain and digestion they are really wanting.
And it’s NOT their fault or your fault.
You’re being told to follow a treatment that has abysmal results in actually healing Celiac disease.
I know, this is hard to believe but I’ll prove it with scientific studies in the next section.
After 2 years on the gluten-free diet, your chances of fully healing your intestines are between 8% and 34%.
2 years of effort for way worse than a coin’s flip chance at healing!
But it only gets worse…
The intestinal leakiness of Celiacs who’d been off gluten for 2 years was found to be 3x more leaky than controls .
WAIT! You might think, “What about those who get symptom-free on a gluten-free diet? Doesn’t that mean all is okay?”
No.
This study and this study looked at inflammation levels in “symptom-free” Celiacs and found significant amounts of inflammation, compared to control subjects.
And it gets even worse, 18 of 30 Celiacs who had been gluten free for 8-12 years, with biopsy-proven health, had poor vitamin status (malnourishment) .
In other words, the gluten-free diet can help you get symptom-free, even repair your villi (proven by biopsy), but it’s unlikely you’ll also repair leaky gut syndrome, reduce inflammation to normal amounts and replace lost nutrients from the malabsorption the disease causes.
It’s time to treat Celiac holistically and use strategies to address the known issues. Yes, you need to avoid the environmental trigger (gluten). But it’s clear that if that’s all you do… well, remember those scary associated conditions like brain, fertility and cancer?
…the Gluten free diet leaves you vulnerable to all of them.
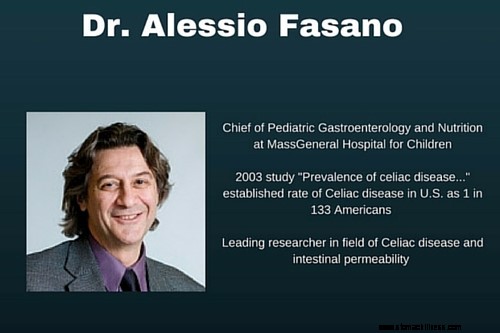
In 2011, Celiac researcher and doctor, Alessio Fasano released his groundbreaking paper, “Leaky Gut and Autoimmune Diseases.” Fasano proposed that this autoimmune attack could actually be stopped!
This is really good news… because, up until this point, it was assumed that once the autoimmune process starts, it’s just going to continue attacking your body for the rest of your life.
But Fasano’s latest research, conducted over several years, has shown that it is indeed possible to stop the attack on the body’s own tissues and usually repair the damage that has happened (if it’s not too beat up).
Fasano’s Theory of Autoimmunity Development Requires 3 Factors:
According to Fasano, when all three of these factors are simultaneously present, autoimmunity develops. This means if you have Celiac or another autoimmune condition, you had to have a leaky gut at the time it started (and it’s likely you still might).
So, this theory finally explains how you could have the genetics for Celiac disease yet remained mostly healthy your whole life. And then BAM! You have a mid-life crisis at 46 that triggers leaky gut, you’re eating gluten and “all of a sudden”you have a full-blown autoimmune disease.
However, there is a silver lining to all of this!
If having a leaky gut is the final factor that allows autoimmune disease to develop, then autoimmune disease can be stopped and most people can heal the damage by fixing the intestinal permeability and removing the trigger (gluten).
This is a whole new way of thinking about Autoimmune disease – one that gives us the steps needed to actually heal the body, instead of becoming another untreated Celiac disease statistic.
It’s also why we now know that while removing gluten (the trigger) is the most important step… it’s not nearly enough to heal a leaky gut and stop the autoimmunity completely. There’s more work to be done before the process has been fully arrested.
Now can you see why the gluten-free diet as the “only treatment” for Celiac disease is just silly?
Here are the 4 steps you need to focus on to actually heal the destruction from Celiac disease. This plan actually takes into account all four of the problems shown in the research to be plaguing Celiac suffers.
This is the plan to heal a leaky gut and reverse the damage from years of untreated Celiac disease…
And it starts with removing gluten from your life. This is still a must!
Step 1 – Remove Gluten (from all food, products, etc.)
It’s time to throw away all the packaged or processed foods in your kitchen that don’t have a gluten-free label on them. There’s no reason to keep any old flour or foods, period. Don’t leave any room for temptation.
You also need to read the labels on any product you put on your skin – shampoo, moisturizer, lotion, chapstick, etc. Ideally, it’s best to think of your skin as a giant extension of your tongue and don’t put anything on it you wouldn’t eat! So, verify that all these products are gluten-free as well.
Next, take a close look at your kitchen hygiene. If there are gluten eaters in the house, you cannot use their non-stick pans (don’t use them, they are toxic), cutting boards, or kitchen utensils. It’s even best to avoid using the same counters. Yes, that is kind of dramatic feeling. But the truth is even trace amounts of gluten can harm you. And if you can’t be safe at home, where you are in control, where can you be?
When you do eat out, don’t be shy about letting your server know of the severity of your condition. To be fully prepared, it’s best to call ahead and verify they can guarantee no cross-contamination. If they can’t guarantee it, there’s a good chance that sooner or later they will serve you some gluten. Here’s a guide to help you eat out gluten-free.
Step 2 – Add Nutritious Foods
It’s clear, from the research, that you need more nutrients than most people and you need to do everything in your power to reduce inflammation.
And this means it’s time to add in some highly-nutritious foods to help replenish the nutrient depletions in your body and give it what it needs to heal. (It costs a lot of nutrients to heal!)
At the same time, these foods will be extremely anti-inflammatory.
It’s a double-whammy move to help you heal.
This means you’ll need to eat A LOT more meat and seafood. It means eating more vegetables, fruits, and naturally starchy foods (sweet potato, white potato, white rice, etc). It means eating more healthy fats, like avocado and coconut products.
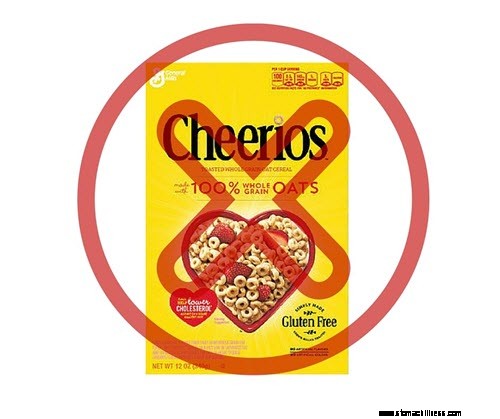
And it means eliminating all grains and pseudograins (even “gluten-free” grains, like corn and oats). Hvorfor? Because these foods have their own “gluten-like” prolamins that wreak havoc in inflamed and damaged guts.
In order to make room for all these new unprocessed and delicious foods, you’ll be eating very little processed gluten-free foods, which will actually save you a bunch of money.
In our experience, the stricter you are to adhering to these rules, the faster you’re likely to heal and feel better.
Step 3 – Heal the Leaky Gut
While cutting out gluten is a pretty straightforward proposal, healing a leaky gut is more complex.
There are endless free tips online on how to heal your leaky gut (some of them are good but many are actually pretty bad), which is why we hired 3 researchers to look at the most current studies and help us figure out the best way to actually do it.
Then, we took these protocols and put them into practice and have seen nothing short of amazing results in 1000’s of people.
One of the first steps to heal a leaky gut is to avoid grains and pseudograins, the ones I told you about in the previous section. Eating the diet above is ideal for healing it.
Next up, you’ll want to try some proven gut-healing supplements, like L-Glutamine. It’s been shown to heal your intestinal mucosa and reduce leaky gut. Start at 2.5 g morning and evening and work up to 20 g morning and night, over two weeks. (Read our complete recommendations on L-Glutamine Do’s and Don’ts.)
With that said, there are 19 triggers of leaky gut and many other helpful supplements out there.
Step 4 – Improve Inflammatory Lifestyles
The last step is used to reduce your inflammation and heal your leaky gut. And it’s all about your lifestyle.
Many Celiacs are unknowingly choosing a lifestyle that creates disease. This includes doing things like going to the gym every day, training for and running marathons, CrossFitting 5 times a week, sleeping less than 7 hours a day, using caffeine after noon, and drinking excess alcohol each night.
Each of these behaviors creates more inflammation and contributes to leaky gut syndrome.
No, don’t freak out! I still want you to work out and exercise, just less strenuously until you’re in better health. I don’t believe that coffee is really bad, but it surely is after noon because it messes up sleep cycles. And I don’t think wine or alcohol is necessarily toxic, but drinking more than one day a week is definitely hurting your gut.
Look, you’re changing your diet, you’re healing your leaky gut, it’s time to take this seriously and that includes cutting out lifestyle habits that are harming you.
Okay, so if you made it this far, you’ll likely be better educated than your doctor on your disease (which is impressive).
Let’s review the important take-home points:
You are now armed with the basic information to really handle and overcome Celiac disease. I hope you share this with others you know who are affected. And let us know in the comments what your number one takeaway from this article is.
Steve
Note:We earn a small commission, if you use the product links on this page to purchase the products we mention. We only recommend products we would use or have used in the past. Your purchase helps support our site and ongoing research.
 Beat Summer Bloat
Betyder sommertid at håndtere sommeroppustethed? Det er almindeligt. Da vi har så lidt tid til virkelig at nyde det gode vejr i Canada, hænger vi vores forklæder op, bruger tid på terrasser, picnic, g
Beat Summer Bloat
Betyder sommertid at håndtere sommeroppustethed? Det er almindeligt. Da vi har så lidt tid til virkelig at nyde det gode vejr i Canada, hænger vi vores forklæder op, bruger tid på terrasser, picnic, g
 Alosetron (Lotronex) effektiv til IBS?
ARKIV FOR LÆGENS VISNINGER Emne:Irritabel tyktarm (IBS), juni 2000 Dr. Lee: Er alosetron effektiv til behandling af IBS? Dr. Mærker : Lotronex er varemærket for alosetron, lægemidlet, som er spe
Alosetron (Lotronex) effektiv til IBS?
ARKIV FOR LÆGENS VISNINGER Emne:Irritabel tyktarm (IBS), juni 2000 Dr. Lee: Er alosetron effektiv til behandling af IBS? Dr. Mærker : Lotronex er varemærket for alosetron, lægemidlet, som er spe
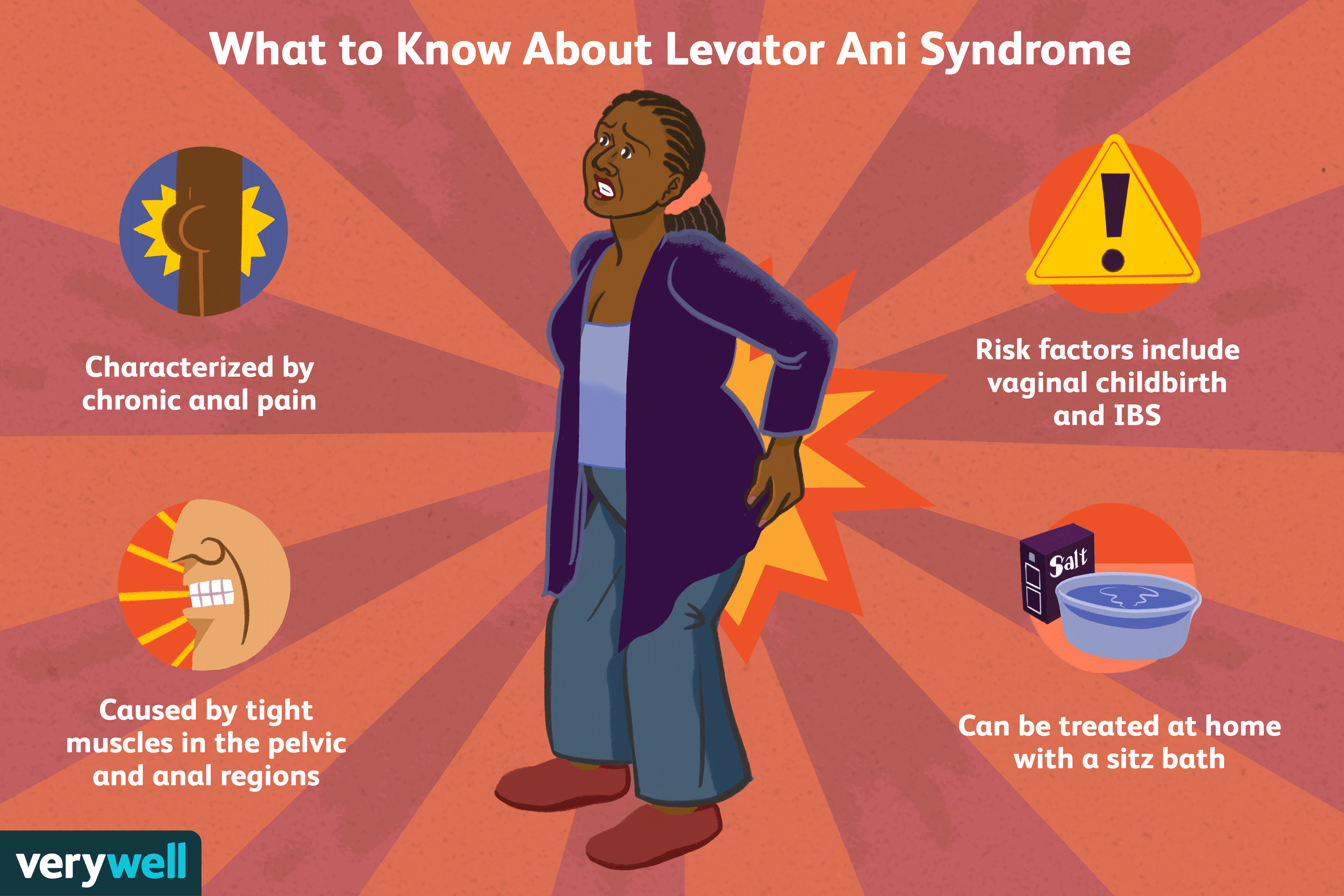 En oversigt over Levator Ani-syndrom
Levator ani syndrom (LAS) er en medicinsk tilstand karakteriseret ved kroniske anale smerter, der er forårsaget af stramme muskler i bækken- og analregionerne. LAS er en af de funktionelle gastroint
En oversigt over Levator Ani-syndrom
Levator ani syndrom (LAS) er en medicinsk tilstand karakteriseret ved kroniske anale smerter, der er forårsaget af stramme muskler i bækken- og analregionerne. LAS er en af de funktionelle gastroint