 Što je HCV, kako se prenosi, postoje li simptomi i je li izlječiv?
Što je HCV, kako se prenosi, postoje li simptomi i je li izlječiv?Većina ljudi koji se zaraze hepatitisom C (hep C) nemaju simptome. Međutim, oni koji imaju simptome mogu doživjeti:
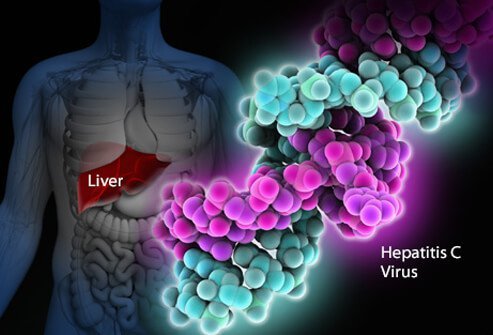
Infekcija virusom hepatitisa C infekcija je jetre uzrokovana virusom hepatitisa C (koji se također naziva HCV ili hep C). Ljudskom imunološkom sustavu teško je eliminirati hepatitis C iz tijela, a infekcija hepatitisom C obično postaje kronična. Tijekom desetljeća, kronična infekcija hepatitisom C oštećuje jetru i može uzrokovati zatajenje jetre. U SAD-u, CDC je procijenio da se 2016. godine dogodilo približno 41.200 novih slučajeva hepatitisa C. Kada virus prvi put uđe u tijelo, obično nema simptoma, pa je ovaj broj procjena. Oko 75% -85% novozaraženih ljudi postaje kronično zaraženo. U SAD-u se procjenjuje da je više od 2 milijuna ljudi kronično zaraženo hepatitisom C. Infekcija se najčešće otkriva među ljudima u dobi od 40 do 60 godina, što odražava visoke stope infekcije u 1970-im i 1980-ima. Svake godine u SAD-u umre 8.000 do 10.000 ljudi povezanih s infekcijom hepatitisom C. HCV infekcija je vodeći uzrok transplantacije jetre u SAD-u i faktor je rizika za rak jetre. U 2016. godini, 18 153 smrtovnice navele su HCV kao uzrok smrti; vjeruje se da je to podcjenjivanje.
Oko 10-20% onih koji razviju kronični HCV razvit će cirozu unutar 20-30 godina. Progresija do ciroze može se ubrzati u dobi iznad 50 godina, muškom spolu, konzumaciji alkohola, nealkoholnoj masnoj bolesti jetre (NASH), koinfekciji s hepatitisom B ili HIV-om i lijekovima za suzbijanje imuniteta. HCV infekcija vodeći je uzrok transplantacije jetre zbog zatajenja jetre u SAD-u
Oni koji imaju cirozu od HCV-a također imaju godišnji rizik od raka jetre (hepatoma ili hepatocelularnog karcinoma) od oko 1%-5%.
Hepatitis znači upalu jetre. Hepatitis C je jedan od nekoliko virusa koji mogu uzrokovati virusni hepatitis. Nije povezan s drugim uobičajenim virusima hepatitisa (na primjer, hepatitisom A ili hepatitisom B). Hepatitis C je član Flaviviridae obitelj virusa. Ostali članovi ove obitelji virusa uključuju one koji uzrokuju žutu groznicu i denga groznicu.
Postoji najmanje šest različitih genotipova (sojeva) virusa koji imaju različite genetske profile (genotipovi 1 do 6). U SAD-u, genotip 1 je najčešći soj hepatitisa C. Čak i unutar jednog genotipa mogu postojati neke varijacije (genotip 1a i 1b, na primjer). Genotipizacija se koristi za usmjeravanje liječenja jer neki virusni genotipovi bolje reagiraju na neke terapije nego na druge.
Poput virusa ljudske imunodeficijencije (HIV), hepatitis C se vrlo brzo razmnožava i postiže vrlo visoke razine u tijelu. Geni koji čine površinske proteine virusa također brzo mutiraju (mijenjaju se), a dnevno se proizvode tisuće genetskih varijacija virusa ("kvazi-vrste"). Tijelo je nemoguće održati korak s stvaranjem anti-HCV protutijela protiv svih kvazi-vrsta koje kruže u isto vrijeme. Još uvijek nije bilo moguće razviti učinkovito cjepivo jer cjepivo mora štititi od svih genotipova.
Infekcija hepatitisom C u jetri pokreće imunološki sustav, što dovodi do upale. Oko 20% -30% akutno zaraženih iskusit će tipične simptome hepatitisa kao što su bol u trbuhu, žutica, tamni urin ili stolica boje gline. Međutim, kronični hepatitis C obično ne uzrokuje simptome sve do vrlo kasne faze bolesti, a hepatitis C je od strane oboljelih nazvan "uspavani zmaj". Tijekom nekoliko godina ili desetljeća, kronična upala može uzrokovati smrt jetrenih stanica i ožiljke ("fibrozu"). Opsežni ožiljci na jetri nazivaju se ciroza. To progresivno narušava vitalne funkcije jetre. Cirotične jetre su sklonije raku jetre. Konzumacija alkohola ubrzava oštećenje jetre s hepatitisom C. Istodobna infekcija HIV-om, kao i akutna infekcija hepatitisom A ili B, također će ubrzati napredovanje u cirozu.
Oko 70% -80% ljudi nema simptome kada prvi put dobiju HCV infekciju. Preostalih 20% -30% možda ima
Rani simptomi hepatitisa C mogu uključivati tamni urin, žute oči ili stolicu boje gline, iako je to neobično. Tijekom vremena, ljudi s kroničnom infekcijom HCV-om mogu razviti znakove upale jetre što sugerira da bi infekcija mogla biti prisutna. Zaražene osobe mogu se lako umoriti ili se žaliti na nespecifične simptome. Kasniji simptomi i znakovi ciroze često izostaju sve dok upala prilično ne uznapreduje. Kako ciroza napreduje, simptomi i znakovi se povećavaju i mogu uključivati:
Budući da se hepatitis C prenosi putem krvi, ne postoji određeno razdoblje zaraznosti. Ljudi koji razviju kronični hepatitis C nose virus u svojoj krvi i stoga su zarazni za druge cijeli život, osim ako se ne izliječe od hepatitisa C.
Teško je sa sigurnošću reći koje je razdoblje inkubacije za hepatitis C, jer većina ljudi koji su zaraženi hepatitisom C nemaju simptome rano u tijeku infekcije. Oni koji razviju simptome rano nakon zaraze (u prosjeku 2 do 12 tjedana, ali mogu biti i dulje) imaju blage gastrointestinalne simptome koji možda neće potaknuti posjet liječniku.
Većina znakova i simptoma infekcije hepatitisom C odnosi se na jetru. Rjeđe, infekcija hepatitisom C može zahvatiti druge organe osim jetre.
Infekcija hepatitisom C može uzrokovati da tijelo proizvodi abnormalna antitijela nazvana krioglobulini. Krioglobulini uzrokuju upalu arterija (vaskulitis). To može oštetiti kožu, zglobove i bubrege. Bolesnici s krioglobulinemijom (krioglobulini u krvi) mogu imati
Osim toga, zaražene osobe s krioglobulinemijom mogu razviti Raynaudov fenomen u kojem prsti na rukama i nogama postaju obojeni (bijeli, zatim ljubičasti, pa crveni) i postaju bolni na niskim temperaturama.
Radna skupina američke preventivne zdravstvene službe preporučuje da se sve odrasle osobe rođene između 1945. i 1965. jednom rutinski testiraju na hepatitis C, bez obzira na to jesu li prisutni čimbenici rizika za hepatitis C. Jednokratno testiranje također se preporučuje za:
Osobe koje su možda bile izložene hepatitisu C u prethodnih 6 mjeseci trebale bi se testirati na opterećenje virusne RNA umjesto anti-HCV antitijela, jer antitijela možda neće biti prisutna do 12 tjedana ili duže nakon infekcije, iako se HCV RNA može otkriti u krvi već 2-3 tjedna nakon infekcije.
Općenito, godišnji probir može biti prikladan za osobe s stalnim čimbenicima rizika kao što su ponovljene spolno prenosive bolesti (STD) ili mnogi seksualni partneri, kontinuirano uzimanje IV droga ili dugotrajni seksualni partneri osoba s hepatitisom C. Treba li testirati ili ne ti se ljudi određuju na temelju odluke od slučaja do slučaja.
Postoji 4% -7% rizik od prijenosa HCV-a s majke na dojenče u svakoj trudnoći. Trenutno ne postoji preporuka CDC-a za rutinski probir hepatitisa C tijekom trudnoće, a trenutno ne postoji ni preporučeni lijek za sprječavanje prijenosa s majke na dojenče (profilaksa). Međutim, CDC prati nalaze istraživanja i može dati preporuke u budućnosti kako se pojave dokazi.
Iako su podaci još uvijek ograničeni, nedavna studija od preko 1.000 slučajeva u Ujedinjenom Kraljevstvu pokazala je da je 11% dojenčadi bilo zaraženo pri rođenju i da je vjerojatno da će ta djeca razviti cirozu u ranim 30-ima. Slučaj probira na HCV tijekom trudnoće uključuje mogućnost sigurnog liječenja majki tijekom trudnoće antivirusnim agensima izravnog djelovanja (DAA) za liječenje majke prije razvoja ciroze, sprječavanje prijenosa dojenčadi i sprječavanje prijenosa na druge. Djeci rođenoj od majki zaraženih HCV-om također se može ponuditi liječenje u ranoj dobi kako bi se spriječila ciroza, kao i prijenos na druge. Koordinacija skrbi između više stručnjaka bit će važna za postizanje ovih ciljeva.
Djeca majki zaraženih HCV-om mogu se testirati na hepatitis C već u dobi od 1-2 mjeseca pomoću virusnog opterećenja hepatitisa C ili PCR testiranja (pogledajte Testovi krvi za hepatitis C). Protutijela na hepatitis C koja se prenose s majke na dijete bit će prisutna do 18 mjeseci, tako da djecu treba testirati na antitijela na HCV ne ranije od ovoga.
Hepatitis C liječi ili gastroenterolog, hepatolog (gastroenterolog s dodatnom obukom za bolesti jetre) ili specijalist za zarazne bolesti. Tim za liječenje može uključivati više od jednog stručnjaka, ovisno o opsegu oštećenja jetre. Kirurzi koji su specijalizirani za kirurgiju jetre, uključujući transplantaciju jetre, dio su medicinskog tima i trebali bi primati pacijente s uznapredovalom bolešću (zatajenje jetre ili ciroza) rano, prije nego što pacijentu treba transplantacija jetre. Možda će moći identificirati probleme koje je potrebno riješiti prije nego što se razmotri operacija. Druge osobe koje mogu biti od pomoći u liječenju pacijenata uključuju dijetetičare koji se savjetuju o pitanjima prehrane i farmaceute koji pomažu u liječenju lijekova.
Postoji nekoliko krvnih pretraga za dijagnozu infekcije hepatitisom C. Krv se može testirati na antitijela na hepatitis C (anti-HCV protutijela). Prosječno je potrebno oko 8-12 tjedana i do 6 mjeseci da se antitijela razviju nakon početne infekcije hepatitisom C, tako da probir na antitijela može propustiti nekoliko novozaraženih osoba. Imati antitijela nije apsolutni pokazatelj aktivnog virusa hepatitisa C koji se razmnožava, ali ako je test na antitijela pozitivan (antitijela su prisutna), statistička vjerojatnost aktivne infekcije je veća od 99%.
Dostupno je nekoliko testova za mjerenje količine virusa hepatitisa C u krvi osobe (virusno opterećenje). RNA virusa hepatitisa C može se identificirati vrstom testa koji se zove lančana reakcija polimeraze (PCR) koji otkriva cirkulirajući virus u krvi već 2-3 tjedna nakon infekcije, tako da se može koristiti za otkrivanje sumnje na akutnu infekciju hepatitisom C rana infekcija. Također se koristi za određivanje je li aktivni hepatitis prisutan kod nekoga tko ima antitijela na hepatitis C i za praćenje virusnog opterećenja tijekom liječenja.
Također se provode krvne pretrage kako bi se identificirali genotipovi HCV-a. Genotipovi različito reagiraju na različite tretmane, stoga su ove informacije važne za odabir najprikladnijeg režima liječenja.
Procjena fibroze jetre pomoću krvnih pretraga također je prilično pouzdana u dijagnosticiranju klinički značajnih ožiljaka; to uključuje FIB-4, FibroSure, Fibrotest i indeks omjera aspartat aminotransferaze-trombocita (APRI).
Sljedeći korak je određivanje razine ožiljaka na jetri do kojih je došlo. Biopsija jetre omogućuje pregled malog uzorka jetrenog tkiva pod mikroskopom, međutim, biopsija jetre je invazivan test i ima značajan rizik od krvarenja. Također može propustiti abnormalna područja u ranoj fazi bolesti.
Neinvazivni testovi uvelike su zamijenili biopsiju jetre osim u posebnim situacijama. Ukočenost jetre ukazuje da mogu biti prisutni uznapredovali ožiljci ili ciroza jetre. Prolazna elastografija može se koristiti za mjerenje ove krutosti ultrazvukom ili magnetskom rezonancijom (MRI).
Evaluacija hepatitisa C prije liječenja također bi trebala uključivati:
Interferons, for example, Roferon-A and Infergen, and pegylated interferons such as Peg-Intron T , Pegasys, were mainstays of treatment for years. Interferons produced sustained viral response (SVR, or cure) of up to 15%. Later, peglatedll forms produced SVR of 50%-80%. These drugs were injected, had many adverse effects, required frequent monitoring, and were often combined with oral ribavirin, which caused anemia. Treatment durations ranged up to 48 weeks.
Direct-acting anti-viral agents (DAAs) are antiviral drugs that act directly on hepatitis C multiplication.
Hepatitis C treatment is best discussed with a doctor or specialist familiar with current and developing options as this field is changing, and even major guidelines may become outdated quickly.
The latest treatment guidelines by the American Association for the Study of Liver Disease (AASLD) and Infectious Disease Society of America (IDSA) recommends use of DAAs as first-line treatment for hepatitis C infection. The choice of DAA varies by specific virus genotype, and the presence or absence of cirrhosis. In the U.S., specific insurance providers also might influence the choice due to the high cost of DAAs. Although the individual, public health, and cost benefits of treating all patients with hepatitis C is clear, the most difficult barrier to treating all people with HCV is the very high cost of the drug regimens. Patients are encouraged to discuss options with their health care professional.
Treatment is recommended in all patients with chronic hepatitis C unless they have a short life expectancy that is not related to liver disease. Severe life-threatening liver disease may require liver transplantation. Newer therapies with DAAs have allowed more and more patients to be treated.
The ultimate goals of antiviral therapy are to
A side goal is preventing co-infections with other hepatitis viruses, such as A and B, which can cause more liver disease than HCV alone. These can be prevented by vaccines and treatment.
When people first get hepatitis C, the infection is said to be acute. Most people with acute hepatitis C do not have symptoms so they are not recognized as being infected. However, some have low-grade fever, fatigue or other symptoms that lead to an early diagnosis. Others who become infected and have a known exposure to an infected source, such as a needlestick injury, are monitored closely.
Treatment decisions should be made on a case-by-case basis. Response to treatment is higher in acute hepatitis infection than chronic infection. However, many experts prefer to hold off treatment for 8-12 weeks to see whether the patient naturally eliminates the virus without treatment. Approaches to treatment are evolving. Patients with acute hepatitis C infection should discuss treatment options with a health care professional who is experienced in treating the disease. There is no established treatment regimen at this time.
If the hepatitis C RNA remains undetectable at the end of the treatment and follow-up period, this is called a sustained virologic response (SVR) and is considered a cure. Over 90% of people treated with DAAs are cured. These people have significantly reduced liver inflammation, and liver scarring may even be reversed.
About 5% of people who are treated for HCV infection are not cured by some of the older regimens. These people may still have options for cure with the newer regimens.
Few people with hepatitis C are at risk for problems if they are treated, however there are some factors that affect treatment regimens, such as concurrent HIV medications and kidney dysfunction. Some drugs are not safe for people with cirrhosis. Individuals who are unable to comply with the treatment schedule for psychological reasons or ongoing drug or alcohol abuse may not be good candidates for treatment because the drugs are very costly and require adherence to the pill regimen and regular follow-up visits. There are some important drug interactions with some of the medications that should be considered by the health care professional.
People with past hepatitis B or who have chronic active hepatitis B should not be treated for HCV without treating for HBV as well. As highly effective treatment for HCV has emerged, reports of serious hepatitis B have come to light. Similar to HCV, hepatitis B usually does not clear from the liver after acute infection, even though it is far less likely to cause chronic active hepatitis than hepatitis C infection. It remains dormant in most people, but it can reactivate with changes in the immune system. It is not clear why eliminating the HCV can allow the HBV infection to flare up. Hepatitis B screening is an important part of the hepatitis C evaluation. Those who have laboratory evidence of active or past infection with HBV should be monitored while receiving HCV treatment.
Compared to interferons and ribavirin drugs, the side effects of DAAs are far fewer and more tolerable. These side effects usually do not require discontinuation of therapy and are self-limiting after completion of therapy.
Patients with hepatitis B co-infection should be monitored for symptoms of reactivation of hepatitis, which are the same as the symptoms of acute hepatitis. The treating doctor may perform blood screening for this as well.
Hepatitis C is the leading reason for 40% to 45% of liver transplants in the U.S. Hepatitis C usually recurs after transplantation and infects the new liver. Approximately 25% of these patients with recurrent hepatitis will develop cirrhosis within five years of transplantation. Despite this, the five-year survival rate for patients with hepatitis C is similar to that of patients who are transplanted for other types of liver disease.
Most transplant centers delay therapy until recurrent hepatitis C in the transplanted liver is confirmed. Oral, highly effective, direct-acting antivirals have shown encouraging results in patients who have undergone liver transplantation for hepatitis C infection and have recurrent hepatitis C. The choice of therapy needs to be individualized and is rapidly evolving.
Once patients successfully complete treatment, the viral load after treatment determines if there is an SVR or cure. If cure is achieved (undetectable viral load after treatment), no further additional testing is recommended unless the patient has cirrhosis. Those who are not cured will need continued monitoring for progression of liver disease and its complications.
While cure eliminates worsening of fibrosis by hepatitis C, complications may still affect those with cirrhosis. These individuals still need regular screening for liver cancer as well as monitoring for esophageal varices that may bleed.
Because hepatitis B co-infection may reactivate or worsen even after treatment for HCV, monitoring for hepatitis symptoms may be needed after the end of therapy.
At this time there are no effective home or over-the-counter treatments for hepatitis C.
Over several years or decades, chronic inflammation may cause death of liver cells and cirrhosis (scaring, fibrosis). When the liver becomes cirrhotic, it becomes stiff, and it cannot perform its normal functions of clearing waste products from the blood. As fibrosis worsens, symptoms of liver failure begin to appear. This is called "decompensated cirrhosis " or "end-stage liver disease. " Symptoms of end-stage liver disease include:
The liver and spleen have an important function of clearing bacteria from the blood stream. Cirrhosis affects many areas of immune function, including attraction of white blood cells to bacteria, reduced killing of bacteria, reduced production of proteins involved in immune defenses, and decreased life span of white blood cells involved in immune defenses. This may be referred to as having cirrhosis-associated immune dysfunction syndrome or CAIDS.
Transmission of hepatitis C can be prevented in several ways.
Prevention programs aim at needle sharing among drug addicts. Needle exchange programs and education have reduced transmission of hepatitis C infection. However, IV drug users are a difficult to reach population, and rates of hepatitis C remain high among them.
Among health care workers, safe needle-usage techniques have been developed to reduce accidental needlesticks. Newer needle systems prevent manual recapping of needles after use of syringes, which is a frequent cause of accidental needlesticks
There is no clear way to prevent hepatitis C transmission from mother to fetus at this time.
People with multiple sexual partners should use barrier precautions such as condoms to limit the risk of hepatitis C and other sexually transmitted diseases, including HIV.
If one partner is infected, monogamous couples may want to consider the low risk of transmission of hepatitis C infection when deciding whether to use condoms during sex. Some couples may decide to use them and some may not.
Screening of the blood supply has almost eliminated the risk of transmission of hepatitis C infection through transfusion.
People with hepatitis C infection should not share razors or toothbrushes with others because of the possibility that these items may be contaminated with blood.
People who want to get a body piercing(s) or tattoo(s) are encouraged to do so only at licensed piercing and tattoo shops (facilities), and verify that the body piercing or tattoo shop uses infection-control practices.
It is critical that physicians and clinics follow manufacturers and regulatory agency directions for sterilizing/cleaning instruments and that disposable instruments be discarded properly. There is no need to use special isolation procedures when dealing with hepatitis C infected patients.
In general, among patients with untreated hepatitis C:
Drinking alcohol and acquiring other hepatitis viruses are risk factors for worse liver disease. People with chronic hepatitis C should avoid drinking alcohol and should be screened for antibodies to hepatitis A and B. If they do not have antibodies, they should be vaccinated against these other hepatitis viruses.
People with hepatitis C should be educated about preventing HIV infection. Infection with both HIV and hepatitis C speeds up and worsens liver damage caused by hepatitis C. Hepatitis C also can affect the HIV infection and how it is treated. About 25% of people with HIV infection are co-infected (also infected) with hepatitis C, and up to 90% of IV drug users with HIV are co-infected with hepatitis C. Screening for hepatitis viruses is important in all people infected with HIV, just as screening for HIV is important in people who have hepatitis C.
Liver cancer (hepatocellular carcinoma, or hepatoma) is associated with cirrhosis from chronic hepatitis C. Some experts recommend screening patients with hepatitis C infection and cirrhosis for liver cancer periodically.
As our knowledge of hepatitis C increases, more and more patients are being diagnosed with chronic infection. Current research is very active and includes diagnosis, natural history, treatment, and vaccine development. Thus the field is constantly changing, with new guidelines added frequently.
 Bolovi u trbuhu u djetinjstvu mogu biti povezani s anksioznošću, depresijom odraslih
Najnovije vijesti o mentalnom zdravlju Više ljudi se uspinje kad je lonac legalan Hoće li vas čitanje knjiga učiniti sretnijim? Zoom Meeting Anksioznost ne pogađa svakoga Slaba akcija na klimatske pr
Bolovi u trbuhu u djetinjstvu mogu biti povezani s anksioznošću, depresijom odraslih
Najnovije vijesti o mentalnom zdravlju Više ljudi se uspinje kad je lonac legalan Hoće li vas čitanje knjiga učiniti sretnijim? Zoom Meeting Anksioznost ne pogađa svakoga Slaba akcija na klimatske pr
 Izbjegavanje sjedilačkog ponašanja:kretanje kako biste ostali zdravi
Ova prošla godina dovela je do toga da ja i moja obitelj živimo više nego ikad. Ova globalna pandemija nas je sve uspaničila i zamrznula na mjestu više od godinu dana. Zajedno s radom od kuće i ograni
Izbjegavanje sjedilačkog ponašanja:kretanje kako biste ostali zdravi
Ova prošla godina dovela je do toga da ja i moja obitelj živimo više nego ikad. Ova globalna pandemija nas je sve uspaničila i zamrznula na mjestu više od godinu dana. Zajedno s radom od kuće i ograni
 IBS okidači koji nisu FODMAP-ovi
Jeste li se ikada zapitali zašto, unatoč savršenom pridržavanju prehrane s niskim FODMAP-om, još uvijek imate simptome IBS-a? IBS je složeno stanje u kojem dijeta s niskim sadržajem FODMAP-a može POM
IBS okidači koji nisu FODMAP-ovi
Jeste li se ikada zapitali zašto, unatoč savršenom pridržavanju prehrane s niskim FODMAP-om, još uvijek imate simptome IBS-a? IBS je složeno stanje u kojem dijeta s niskim sadržajem FODMAP-a može POM