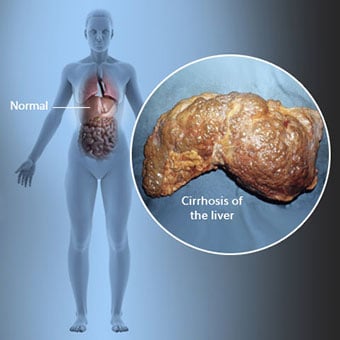
 Skrumpelever er en komplikation af leversygdom, der involverer tab af leverceller og irreversibel ardannelse i leveren.
Skrumpelever er en komplikation af leversygdom, der involverer tab af leverceller og irreversibel ardannelse i leveren. Personer med skrumpelever kan have få eller ingen symptomer og tegn på leversygdom. Nogle af symptomerne kan være uspecifikke, det vil sige, at de ikke tyder på, at leveren er deres årsag. Nogle af de mere almindelige symptomer og tegn på skrumpelever inkluderer:
Personer med skrumpelever udvikler også symptomer og tegn fra komplikationer af skrumpelever.
 Der er mange årsager til skrumpelever, herunder kemikalier (såsom alkohol, fedt og visse medikamenter), vira, giftige metaller, og autoimmun leversygdom, hvor kroppens immunsystem angriber leveren.
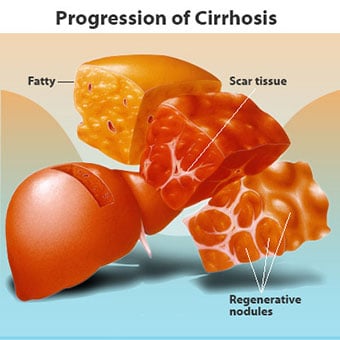
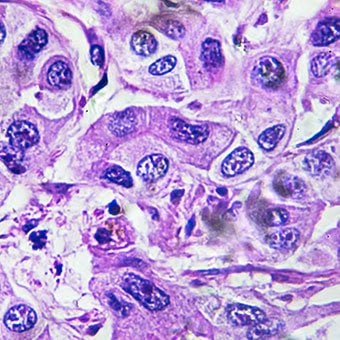
Der er mange årsager til skrumpelever, herunder kemikalier (såsom alkohol, fedt og visse medikamenter), vira, giftige metaller, og autoimmun leversygdom, hvor kroppens immunsystem angriber leveren. Skrumpelever er en komplikation af mange leversygdomme karakteriseret ved unormal leverstruktur og funktion. De sygdomme, der fører til skrumpelever, gør det, fordi de skader og dræber leverceller, hvorefter den betændelse og reparation, der er forbundet med de døende leverceller, får arvæv til at dannes. De leverceller, der ikke dør, formerer sig i et forsøg på at erstatte de celler, der er døde. Dette resulterer i klynger af nydannede leverceller (regenerative knuder) i arvævet. Der er mange årsager til skrumpelever, herunder kemikalier (såsom alkohol, fedt og visse lægemidler), vira, giftige metaller (såsom jern og kobber, der ophobes i leveren som følge af genetiske sygdomme) og autoimmun leversygdom, hvor kroppens immunsystem angriber leveren.
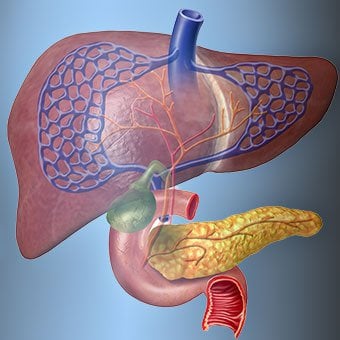
 Forholdet mellem leveren og blodet er unikt.
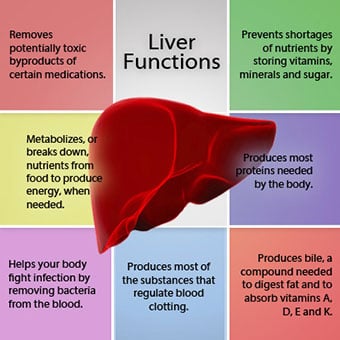
Forholdet mellem leveren og blodet er unikt. Leveren er et vigtigt organ i kroppen. Det udfører mange kritiske funktioner, hvoraf to er at producere stoffer, som kroppen kræver, for eksempel at størkne proteiner, der er nødvendige for at blodet kan størkne, og at fjerne giftige stoffer, der kan være skadelige for kroppen, f.eks. . Leveren har også en vigtig rolle i at regulere tilførslen af glukose (sukker) og lipider (fedt), som kroppen bruger som brændstof. For at kunne udføre disse kritiske funktioner skal levercellerne fungere normalt, og de skal have en tæt nærhed til blodet, fordi de stoffer, der tilføres eller fjernes af leveren, transporteres til og fra leveren med blodet.
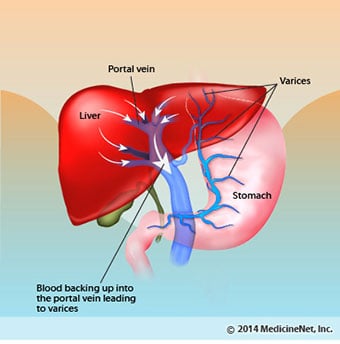
Forholdet mellem leveren og blodet er unikt. I modsætning til de fleste organer i kroppen, tilføres kun en lille mængde blod til leveren via arterier. Det meste af leverens blodforsyning kommer fra tarmvenerne, når blodet vender tilbage til hjertet. Hovedvenen, der returnerer blod fra tarmene, kaldes portvenen. Når portvenen passerer gennem leveren, bryder den op i stadig mindre og mindre vener. De mindste årer (kaldet sinusoider på grund af deres unikke struktur) er i tæt kontakt med levercellerne. Leverceller stiller op langs sinusoiderne. Dette tætte forhold mellem levercellerne og blod fra portvenen gør det muligt for levercellerne at fjerne og tilføje stoffer til blodet. Når blodet er gået gennem sinusoiderne, opsamles det i stadig større og større vener, der i sidste ende danner en enkelt vene, levervenen, som returnerer blodet til hjertet.
Ved skrumpelever ødelægges forholdet mellem blod og leverceller. Selvom de leverceller, der overlever eller er nydannet, måske er i stand til at producere og fjerne stoffer fra blodet, har de ikke det normale, intime forhold til blodet, og det forstyrrer levercellernes evne til at tilføje eller fjerne stoffer. fra blodet. Derudover hindrer ardannelsen i den skrumpelever strømmen af blod gennem leveren og til levercellerne. Som et resultat af obstruktionen af strømmen af blod gennem leveren "back-up" blodet i portvenen, og trykket i portvenen stiger, en tilstand kaldet portal hypertension. På grund af forhindring af flow og høje tryk i portvenen søger blodet i portvenen andre vener, hvori de kan vende tilbage til hjertet, vener med lavere tryk, der går uden om leveren. Desværre er leveren ikke i stand til at tilføje eller fjerne stoffer fra blod, der omgår den. Det er en kombination af reduceret antal leverceller, tab af den normale kontakt mellem blod, der passerer gennem leveren og levercellerne, og blod, der går uden om leveren, der fører til mange af tegnene på skrumpelever.
En anden grund til problemerne forårsaget af skrumpelever er det forstyrrede forhold mellem levercellerne og de kanaler, gennem hvilke galden strømmer. Galde er en væske produceret af leverceller, der har to vigtige funktioner:at hjælpe med fordøjelsen og at fjerne og fjerne giftige stoffer fra kroppen. Galden produceret af leverceller udskilles i meget små kanaler, der løber mellem levercellerne, der beklæder sinusoiderne, kaldet canaliculi. Canaliculi udmunder i små kanaler, som derefter går sammen og danner større og større kanaler. Alle kanalerne kombineres i en kanal, der kommer ind i tyndtarmen, hvor den kan hjælpe med fordøjelsen af maden. På samme tid kommer giftige stoffer indeholdt i galden ind i tarmen og elimineres derefter i afføringen. Ved skrumpelever er canaliculi unormale, og forholdet mellem leverceller og canaliculi er ødelagt, ligesom forholdet mellem levercellerne og blod i sinusoiderne. Som et resultat er leveren ikke i stand til at eliminere giftige stoffer normalt, og de kan ophobes i kroppen. I mindre grad er fordøjelsen i tarmen også nedsat.
 Almindelige symptomer og tegn på skrumpelever omfatter gulsot, træthed, svaghed, appetitløshed, kløe og let blå mærker.
Almindelige symptomer og tegn på skrumpelever omfatter gulsot, træthed, svaghed, appetitløshed, kløe og let blå mærker. Mennesker med skrumpelever kan have få eller ingen symptomer og tegn på leversygdom. Nogle af symptomerne kan være uspecifikke og tyder ikke på, at leveren er deres årsag. Almindelige symptomer og tegn på skrumpelever omfatter:
Mennesker med skrumpelever, hvis leveren også udvikler symptomer og tegn fra sygdommens komplikationer.
Cirrhose i sig selv er allerede et sent stadium af leverskade. I de tidlige stadier af leversygdomme vil der være betændelse i leveren. Hvis denne betændelse ikke behandles, kan det føre til ardannelse (fibrose). På dette stadium er det stadig muligt for leveren at hele med behandling.
Hvis fibrose i leveren ikke behandles, kan det resultere i skrumpelever. På dette stadium kan arvævet ikke heles, men progressionen af ardannelsen kan forhindres eller bremses. Mennesker med skrumpelever, der har tegn på komplikationer, kan udvikle leversygdom i slutstadiet (ESLD), og den eneste behandling på dette stadium er levertransplantation.
 Ødem, ascites og bakteriel peritonitis komplikationer
Ødem, ascites og bakteriel peritonitis komplikationer Efterhånden som skrumpelever bliver alvorlig, sendes der signaler til nyrerne om at tilbageholde salt og vand i kroppen. Det overskydende salt og vand samler sig først i vævet under huden på anklerne og benene på grund af tyngdekraftens virkning, når du står eller sidder. Denne ophobning af væske kaldes perifert ødem eller pitting ødem. (Pitting ødem refererer til det faktum, at et tryk af en fingerspids fast mod en ankel eller et ben med ødem forårsager en fordybning i huden, der varer ved i nogen tid efter udløsning af trykket. Enhver form for tryk, såsom fra elastikken på en strømpe , kan være nok til at forårsage pitting.) Hævelsen er ofte værre i slutningen af en dag efter at have stået eller siddende og kan aftage natten over, når du ligger ned. Efterhånden som skrumpelever forværres og mere salt og vand tilbageholdes, kan væske også samle sig i bughulen mellem bugvæggen og bugorganerne (kaldet ascites), hvilket forårsager hævelse af maven, ubehag i maven og øget vægt.
Væske i bughulen (ascites) er det perfekte sted for bakterier at vokse. Normalt indeholder bughulen en meget lille mængde væske, der godt kan modstå infektion, og bakterier, der kommer ind i maven (normalt fra tarmen), dræbes eller finder vej ind i portvenen og til leveren, hvor de bliver dræbt. Ved skrumpelever er væsken, der samler sig i maven, ikke i stand til at modstå infektion normalt. Derudover finder flere bakterier vej fra tarmen til ascites. Infektion i maven og ascites, kaldet spontan bakteriel peritonitis eller SBP, vil sandsynligvis forekomme. SBP er en livstruende komplikation. Nogle patienter med SBP har ingen symptomer, mens andre har feber, kulderystelser, mavesmerter og ømhed, diarré og forværret ascites.
 Blødning og miltkomplikationer
Blødning og miltkomplikationer I skrumpelever blokerer arvævet for strømmen af blod, der vender tilbage til hjertet fra tarmene og øger trykket i portvenen (portal hypertension). Når trykket i portvenen bliver højt nok, får det blod til at strømme rundt i leveren gennem vener med lavere tryk for at nå hjertet. De mest almindelige vener, hvorigennem blodet passerer leveren, er venerne, der beklæder den nederste del af spiserøret og den øverste del af maven.
Som et resultat af den øgede blodgennemstrømning og den resulterende stigning i tryk, udvider venerne i den nedre spiserør og øvre mave sig og omtales derefter som esophageal og gastriske varicer; jo højere portaltrykket er, jo større er varicerne, og jo mere sandsynligt er det, at en patient bløder fra varicerne ind i spiserøret eller maven.
Blødning fra varicer er alvorlig og kan uden øjeblikkelig behandling være dødelig. Symptomer på blødning fra varicer omfatter opkastning af blod (det kan se ud som rødt blod blandet med blodpropper eller "kaffegrums"), afføring, der er sort og tjæreagtig på grund af ændringer i blodet, når det passerer gennem tarmen (melena) og ortostatisk afføring. svimmelhed eller besvimelse (forårsaget af et fald i blodtrykket, især når man rejser sig op fra en liggende stilling).
Blødning kan sjældent forekomme fra varicer, der dannes andre steder i tarmene, for eksempel tyktarmen. Patienter indlagt på hospitalet på grund af aktivt blødende esophagusvaricer har en høj risiko for at udvikle spontan bakteriel peritonitis, selvom årsagerne hertil endnu ikke er forstået.
Milten fungerer normalt som et filter til at fjerne ældre røde blodlegemer, hvide blodlegemer og blodplader (små partikler, der er vigtige for blodets størkning). Blodet, der dræner fra milten, slutter sig til blodet i portvenen fra tarmene. Efterhånden som trykket i portvenen stiger ved skrumpelever, blokerer det i stigende grad blodstrømmen fra milten. Blodet "back-up", akkumuleres i milten, og milten svulmer i størrelse, en tilstand, der omtales som splenomegali. Nogle gange er milten så forstørret, at det forårsager mavesmerter.
Efterhånden som milten forstørres, filtrerer den flere og flere af blodcellerne og blodpladerne ud, indtil deres antal i blodet er reduceret. Hypersplenisme er det udtryk, der bruges til at beskrive denne tilstand, og det er forbundet med et lavt antal røde blodlegemer (anæmi), lavt antal hvide blodlegemer (leukopeni) og/eller et lavt antal blodplader (trombocytopeni). Anæmi kan forårsage svaghed, leukopeni kan føre til infektioner, og trombocytopeni kan svække blodets størkning og resultere i langvarig blødning
 Leverkomplikationer (lever)
Leverkomplikationer (lever) Skrumpelever på grund af enhver årsag øger risikoen for primær leverkræft (hepatocellulært karcinom). Primær refererer til det faktum, at tumoren stammer fra leveren. En sekundær leverkræft er en, der stammer fra andre steder i kroppen og spreder sig (metastaserer) til leveren.
De mest almindelige symptomer og tegn på primær leverkræft er mavesmerter og hævelse, en forstørret lever, vægttab og feber. Derudover kan leverkræft producere og frigive en række stoffer, inklusive dem, der forårsager et øget antal røde blodlegemer (erythrocytosis), lavt blodsukker (hypoglykæmi) og højt blodcalcium (hypercalcæmi).
Noget af det protein i maden, der undslipper fordøjelsen og optagelsen, bruges af bakterier, der normalt er til stede i tarmen. Mens de bruger proteinet til deres egne formål, laver bakterierne stoffer, som de frigiver til tarmen for derefter at blive optaget i kroppen. Nogle af disse stoffer, såsom ammoniak, kan have toksiske virkninger på hjernen. Normalt føres disse giftige stoffer fra tarmen i portvenen til leveren, hvor de fjernes fra blodet og afgiftes.
Når skrumpelever er til stede, kan leverceller ikke fungere normalt, enten fordi de er beskadiget, eller fordi de har mistet deres normale forhold til blodet. Derudover passerer noget af blodet i portvenen leveren gennem andre vener. Resultatet af disse abnormiteter er, at giftige stoffer ikke kan fjernes af levercellerne, og i stedet ophobes i blodet.
Når de giftige stoffer ophobes tilstrækkeligt i blodet, forringes hjernens funktion, en tilstand kaldet hepatisk encefalopati. At sove om dagen i stedet for om natten (vending af det normale søvnmønster) er et tidligt symptom på hepatisk encefalopati. Andre symptomer omfatter irritabilitet, manglende evne til at koncentrere sig eller udføre beregninger, hukommelsestab, forvirring eller nedsatte bevidsthedsniveauer. I sidste ende forårsager alvorlig hepatisk encefalopati koma og død.
De giftige stoffer gør også hjernen hos patienter med skrumpelever meget følsomme over for lægemidler, der normalt filtreres og afgiftes af leveren. Doser af mange lægemidler skal muligvis reduceres for at undgå en giftig opbygning i skrumpelever, især beroligende midler og lægemidler, der bruges til at fremme søvn. Alternativt kan der anvendes lægemidler, som ikke behøver at blive afgiftet eller elimineret fra kroppen af leveren, såsom lægemidler, der elimineres af nyrerne.
Patienter med forværret cirrhose kan udvikle hepatorenalt syndrom. Dette syndrom er en alvorlig komplikation, hvor nyrernes funktion er nedsat. Det er et funktionelt problem i nyrerne, hvilket betyder, at der ikke er nogen fysisk skade på nyrerne. I stedet skyldes den nedsatte funktion ændringer i den måde, blodet strømmer gennem selve nyrerne på. Det hepatorenale syndrom er defineret som nyrernes progressive svigt i at fjerne stoffer fra blodet og producere tilstrækkelige mængder urin, mens andre vigtige funktioner i nyrerne, såsom tilbageholdelse af salt, opretholdes. Hvis leverfunktionen forbedres, eller en sund lever transplanteres til en patient med hepatorenalt syndrom, begynder nyrerne normalt at fungere normalt igen. Dette tyder på, at nyrernes nedsatte funktion er resultatet af enten ophobning af giftige stoffer i blodet eller unormal leverfunktion, når leveren svigter. Der er to typer af hepatorenalt syndrom. En type opstår gradvist over måneder. Den anden opstår hurtigt over en uge eller to.
Sjældent kan nogle patienter med fremskreden cirrhose udvikle hepatopulmonalt syndrom. Disse patienter kan opleve åndedrætsbesvær, fordi visse hormoner, der frigives ved fremskreden skrumpelever, får lungerne til at fungere unormalt. Det grundlæggende problem i lungen er, at der ikke strømmer nok blod gennem de små blodkar i lungerne, som er i kontakt med lungernes alveoler (luftsække). Blod, der strømmer gennem lungerne, shuntes rundt om alveolerne og kan ikke optage nok ilt fra luften i alveolerne. Som følge heraf oplever patienten åndenød, især ved anstrengelse.
 Der er 12 almindelige årsager til skrumpelever.
Der er 12 almindelige årsager til skrumpelever. Almindelige årsager af skrumpelever omfatter:
Less common causes of cirrhosis include:
In certain parts of the world (particularly Northern Africa), infection of the liver with a parasite (schistosomiasis) is the most common cause of liver disease and cirrhosis.
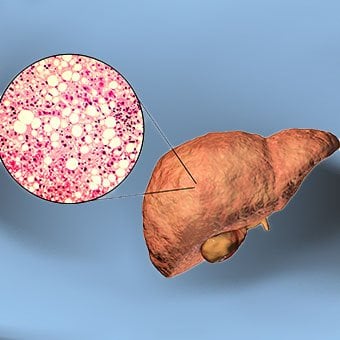 Alcohol and nonalcoholic fatty liver disease are common causes of cirrhosis.
Alcohol and nonalcoholic fatty liver disease are common causes of cirrhosis. Alcohol is a very common cause of cirrhosis, particularly in the Western world. Chronic, high levels of alcohol consumption injure liver cells. Thirty percent of individuals who drink daily at least eight to sixteen ounces of hard liquor or the equivalent for fifteen or more years will develop cirrhosis. Alcohol causes a range of liver diseases, which include simple and uncomplicated fatty liver (steatosis), more serious fatty liver with inflammation (steatohepatitis or alcoholic hepatitis), and cirrhosis.
Nonalcoholic fatty liver disease (NAFLD) refers to a wide spectrum of liver diseases that, like alcoholic liver disease, range from simple steatosis, to nonalcoholic steatohepatitis (NASH), to cirrhosis. All stages of NAFLD have in common the accumulation of fat in liver cells. The term nonalcoholic is used because NAFLD occurs in individuals who do not consume excessive amounts of alcohol, yet in many respects the microscopic picture of NAFLD is similar to what can be seen in liver disease that is due to excessive alcohol. NAFLD is associated with a condition called insulin resistance, which, in turn, is associated with metabolic syndrome and diabetes mellitus type 2. Obesity is the main cause of insulin resistance, metabolic syndrome, and type 2 diabetes. NAFLD is the most common liver disease in the United States and is responsible for up to 25% of all liver disease. The number of livers transplanted for NAFLD-related cirrhosis is on the rise. Public health officials are worried that the current epidemic of obesity will dramatically increase the development of NAFLD and cirrhosis in the population.
 Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women.
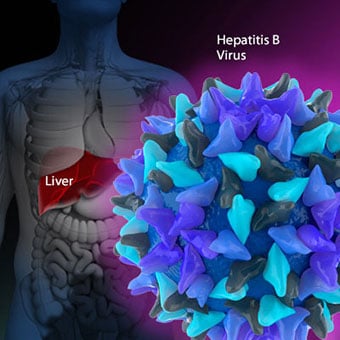
Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women. Chronic viral hepatitis is a condition in which hepatitis B or hepatitis C virus infects the liver for years. Most patients with viral hepatitis will not develop chronic hepatitis and cirrhosis. The majority of patients infected with hepatitis A recover completely within weeks, without developing chronic infection. In contrast, some patients infected with hepatitis B virus and most patients infected with hepatitis C virus develop chronic hepatitis, which, in turn, causes progressive liver damage and leads to cirrhosis, and, sometimes, liver cancers.
Autoimmune hepatitis is a liver disease found more commonly in women that is caused by an abnormality of the immune system. The abnormal immune activity in autoimmune hepatitis causes progressive inflammation and destruction of liver cells (hepatocytes), leading ultimately to cirrhosis.
Primary biliary cirrhosis (PBC) is a liver disease caused by an abnormality of the immune system that is found predominantly in women. The abnormal immunity in PBC causes chronic inflammation and destruction of the small bile ducts within the liver. The bile ducts are passages within the liver through which bile travels to the intestine. Bile is a fluid produced by the liver that contains substances required for digestion and absorption of fat in the intestine, as well as other compounds that are waste products, such as the pigment bilirubin. (Bilirubin is produced by the breakdown of hemoglobin from old red blood cells.). Along with the gallbladder, the bile ducts make up the biliary tract. In PBC, the destruction of the small bile ducts blocks the normal flow of bile into the intestine. As the inflammation continues to destroy more of the bile ducts, it also spreads to destroy nearby liver cells. As the destruction of the hepatocytes proceeds, scar tissue (fibrosis) forms and spreads throughout the areas of destruction. The combined effects of progressive inflammation, scarring, and the toxic effects of accumulating waste products culminates in cirrhosis.
Primary sclerosing cholangitis (PSC) is an uncommon disease frequently found in patients with Crohn's disease and ulcerative colitis. In PSC, the large bile ducts outside of the liver become inflamed, narrowed, and obstructed. Obstruction to the flow of bile leads to infections of the bile ducts and jaundice, eventually causing cirrhosis. In some patients, injury to the bile ducts (usually because of surgery) also can cause obstruction and cirrhosis of the liver.
 Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others.
Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others. Inherited (genetic) disorders that result in the accumulation of toxic substances in the liver, which leads to tissue damage and cirrhosis. Examples include the abnormal accumulation of iron (hemochromatosis) or copper (Wilson disease). In hemochromatosis, patients inherit a tendency to absorb an excessive amount of iron from food. Over time, iron accumulation in different organs throughout the body causes cirrhosis, arthritis, heart muscle damage leading to heart failure, and testicular dysfunction causing loss of sexual drive. Treatment is aimed at preventing damage to organs by removing iron from the body through phlebotomy (removing blood). In Wilson disease, there is an inherited abnormality in one of the proteins that control copper in the body. Over time, copper accumulates in the liver, eyes, and brain. Cirrhosis, tremor, psychiatric disturbances, and other neurological difficulties occur if the condition is not treated early. Treatment is with oral medication, which increases the amount of copper that is eliminated from the body in the urine.
Cryptogenic cirrhosis (cirrhosis due to unidentified causes) is a common reason for liver transplantation. It is termed called cryptogenic cirrhosis because for many years doctors have been being unable to explain why a proportion of patients developed cirrhosis. Doctors now believe that cryptogenic cirrhosis is due to NASH (nonalcoholic steatohepatitis) caused by long-standing obesity, type 2 diabetes, and insulin resistance. The fat in the liver of patients with NASH is believed to disappear with the onset of cirrhosis, and this has made it difficult for doctors to make the connection between NASH and cryptogenic cirrhosis for a long time. One important clue that NASH leads to cryptogenic cirrhosis is the finding of a high occurrence of NASH in the new livers of patients undergoing liver transplant for cryptogenic cirrhosis. Finally, a study from France suggests that patients with NASH have a similar risk of developing cirrhosis as patients with long-standing infection with hepatitis C virus. (See discussion that follows.) However, the progression to cirrhosis from NASH is thought to be slow and the diagnosis of cirrhosis typically is made in people in their sixties.
Infants can be born without bile ducts (biliary atresia) and ultimately develop cirrhosis. Other infants are born lacking vital enzymes for controlling sugars that lead to the accumulation of sugars and cirrhosis. On rare occasions, the absence of a specific enzyme can cause cirrhosis and scarring of the lung (alpha-1 antitrypsin deficiency).
Less common causes of cirrhosis include unusual reactions to some drugs and prolonged exposure to toxins, as well as chronic heart failure (cardiac cirrhosis). In certain parts of the world (particularly Northern Africa), infection of the liver with a parasite (schistosomiasis) is the most common cause of liver disease and cirrhosis.
 Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others.
Different liver diseases should be diagnosed by specialists and different tests such as liver blood test, biopsy, and others. The single best test for diagnosing cirrhosis is a biopsy of the liver. Liver biopsies carry a small risk for serious complications, and biopsy often is reserved for those patients in whom the diagnosis of the type of liver disease or the presence of cirrhosis is not clear. The history, physical examination, or routine testing may suggest the possibility of cirrhosis. If cirrhosis is present, other tests can be used to determine the severity of the cirrhosis and the presence of complications. Tests also may be used to diagnose the underlying disease that is causing the cirrhosis. Examples of how doctors diagnose and evaluate cirrhosis are:
 There are four types of treatment of cirrhosis.
There are four types of treatment of cirrhosis. Treatment of cirrhosis includes
Consume a balanced diet and one multivitamin daily. Patients with PBC with impaired absorption of fat-soluble vitamins may need additional vitamins D and K.
Avoid drugs (including alcohol) that cause liver damage. All patients with cirrhosis should avoid alcohol. Most patients with alcohol-induced cirrhosis experience an improvement in liver function with abstinence from alcohol. Even patients with chronic hepatitis B and C can substantially reduce liver damage and slow the progression towards cirrhosis with abstinence from alcohol.
Avoid nonsteroidal anti-inflammatory drugs (NSAIDs, e.g., ibuprofen). Patients with cirrhosis can experience worsening of liver and kidney function with NSAIDs.
Eradicate hepatitis B and hepatitis C virus by using anti-viral medications. Not all patients with cirrhosis due to chronic viral hepatitis are candidates for drug treatment. Some patients may experience serious deterioration in liver function and/or intolerable side effects during treatment. Thus, decisions to treat viral hepatitis have to be individualized, after consulting with doctors experienced in treating liver diseases (hepatologists).
Remove blood from patients with hemochromatosis to reduce the levels of iron and prevent further damage to the liver. In Wilson's disease, medications can be used to increase the excretion of copper in the urine to reduce the levels of copper in the body and prevent further damage to the liver.
Suppress the immune system with drugs such as prednisone and azathioprine (Imuran) to decrease inflammation of the liver in autoimmune hepatitis.
Treat patients with PBC with a bile acid preparation, ursodeoxycholic acid (UDCA), also called ursodiol (Actigall). Results of an analysis that combined the results from several clinical trials showed that UDCA increased survival among PBC patients during 4 years of therapy. The development of portal hypertension also was reduced by the UDCA. It is important to note that despite producing clear benefits, UDCA treatment primarily retards progression and does not cure PBC. Other medications such as colchicine and methotrexate also may have benefits in subsets of patients with PBC.
Immunize patients with cirrhosis against infection with hepatitis A and B to prevent a serious deterioration in liver. There are currently no vaccines available for immunizing against hepatitis C.
 Treatment for edema, ascites, and hypersplenism complications.
Treatment for edema, ascites, and hypersplenism complications. Retaining salt and water can lead to swelling of the ankles and legs (edema) or abdomen (ascites) in patients with cirrhosis. Doctors often advise patients with cirrhosis to restrict dietary salt (sodium) and fluid to decrease edema and ascites. The amount of salt in the diet usually is restricted to 2 grams per day and fluid to 1.2 liters per day. In most patients with cirrhosis, salt and fluid restriction is not enough and diuretics have to be added.
Diuretics are medications that work in the kidneys to promote the elimination of salt and water into the urine. A combination of the diuretics spironolactone (Aldactone) and furosemide (Lasix) can reduce or eliminate the edema and ascites in most patients. During treatment with diuretics, it is important to monitor the function of the kidneys by measuring blood levels of blood urea nitrogen (BUN) and creatinine to determine if too much diuretic is being used. Too much diuretic can lead to kidney dysfunction that is reflected in elevations of the BUN and creatinine levels in the blood.
Sometimes, when the diuretics do not work (in which case the ascites is said to be refractory), a long needle or catheter is used to draw out the ascitic fluid directly from the abdomen, a procedure called abdominal paracentesis. It is common to withdraw large amounts (liters) of fluid from the abdomen when the ascites is causing painful abdominal distension and/or difficulty breathing because it limits the movement of the diaphragms.
Another treatment for refractory ascites is a procedure called transjugular intravenous portosystemic shunting (TIPS).
The spleen normally acts as a filter to remove older red blood cells, white blood cells, and platelets (small particles important for the clotting of blood). The blood that drains from the spleen joins the blood in the portal vein from the intestines. As the pressure in the portal vein rises in cirrhosis, it increasingly blocks the flow of blood from the spleen. The blood "backs-up," accumulating in the spleen, and the spleen swells in size, a condition referred to as splenomegaly. Sometimes, the spleen is so enlarged it causes abdominal pain.
As the spleen enlarges, it filters out more and more of the blood cells and platelets until their numbers in the blood are reduced. Hypersplenism is the term used to describe this condition, and it is associated with a low red blood cell count (anemia), low white blood cell count (leukopenia), and/or a low platelet count (thrombocytopenia). Anemia can cause weakness, leucopenia can lead to infections, and thrombocytopenia can impair the clotting of blood and result in prolonged bleeding.
 Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding.
Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding. If large varices develop in the esophagus or upper stomach, patients with cirrhosis are at risk for serious bleeding due to rupture of these varices. Once varices have bled, they tend to rebleed and the probability that a patient will die from each bleeding episode is high (30% to 35%). Treatment is necessary to prevent the first bleeding episode as well as rebleeding. Treatments include medications and procedures to decrease the pressure in the portal vein and procedures to destroy the varices.
 Hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose.
Hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose. Patients with an abnormal sleep cycle, impaired thinking, odd behavior, or other signs of hepatic encephalopathy usually should be treated with a low protein diet and oral lactulose. Dietary protein is restricted because it is a source of toxic compounds that cause hepatic encephalopathy. Lactulose, which is a liquid, traps toxic compounds in the colon so they cannot be absorbed into the bloodstream, and thus cause encephalopathy. Lactulose is converted to lactic acid in the colon, and the acidic environment that results is believed to trap the toxic compounds produced by the bacteria. To be sure adequate lactulose is present in the colon at all times, the patient should adjust the dose to produce 2 to 3 semiformed bowel movements a day. Lactulose is a laxative, and the effectiveness of treatment can be judged by loosening or increasing the frequency of stools. Rifaximin (Xifaxan) is an antibiotic taken orally that is not absorbed into the body but rather remains in the intestines. It is the preferred mode of treatment of hepatic encephalopathy. Antibiotics work by suppressing the bacteria that produce the toxic compounds in the colon.
 Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics.
Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics. Patients suspected of having spontaneous bacterial peritonitis usually will undergo paracentesis. The fluid that is removed is examined for white blood cells and cultured for bacteria. Culturing involves inoculating a sample of the ascites into a bottle of nutrient-rich fluid that encourages the growth of bacteria, thus facilitating the identification of even small numbers of bacteria. Blood and urine samples also are often obtained for culturing because many patients with spontaneous bacterial peritonitis also will have infections in their blood and urine. Many doctors believe the infection may have begun in the blood and the urine and spread to the ascitic fluid to cause spontaneous bacterial peritonitis. Most patients with spontaneous bacterial peritonitis are hospitalized and treated with intravenous antibiotics such as cefotaxime (Claforan). Patients usually treated with antibiotics include:
Spontaneous bacterial peritonitis is a serious infection. It often occurs in patients with advanced cirrhosis whose immune systems are weak, but with modern antibiotics and early detection and treatment, the prognosis of recovering from an episode of spontaneous bacterial peritonitis is good.
In some patients, oral antibiotics (norfloxacin [Noroxin] or sulfamethoxazole and trimethoprim [Bactrim]) can be prescribed to prevent spontaneous bacterial peritonitis. Not all patients with cirrhosis and ascites should be treated with antibiotics to prevent spontaneous bacterial peritonitis, but some patients are at high risk for developing spontaneous bacterial peritonitis and warrant preventive treatment.
 The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases.
The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases. Several types of liver disease that cause cirrhosis (such as hepatitis B and C) are associated with a high incidence of liver cancer. It is useful to screen for liver cancer in patients with cirrhosis, as early surgical treatment or transplantation of the liver can cure the patient of cancer. The difficulty is that the methods available for screening are only partially effective, identifying at best only half of patients at a curable stage of their cancer. Despite the partial effectiveness of screening, most patients with cirrhosis, particularly hepatitis B and C, are screened yearly or every six months with ultrasound examination of the liver and measurements of cancer-produced proteins in the blood, for example, alpha-fetoprotein.
Cirrhosis is irreversible. Liver function usually gradually worsens despite treatment, and complications of cirrhosis increase and become difficult to treat. When cirrhosis is far advanced liver transplantation often is the only option for treatment. Recent advances in surgical transplantation and medications to prevent infection and rejection of the transplanted liver have greatly improved survival after transplantation. On average, more than 80% of patients who receive transplants are alive after five years. Not everyone with cirrhosis is a candidate for transplantation. Furthermore, there is a shortage of livers to transplant, and they're usually is a long (months to years) wait before a liver for transplanting becomes available. Measures to slow the progression of liver disease, and treat and prevent complications of cirrhosis are vitally important.
The prognosis and life expectancy for cirrhosis of the liver varies and depends on the cause, the severity, any complications, and any underlying diseases.
Progress in the management and prevention of cirrhosis continues. Research is ongoing to determine the mechanism of scar formation in the liver and how this process of scarring can be interrupted or even reversed. Newer and better treatments for viral liver disease are being developed to prevent the progression to cirrhosis. Prevention of viral hepatitis by vaccination, which is available for hepatitis B, is being developed for hepatitis C. Treatments for the complications of cirrhosis are being developed or revised, and tested continually. Finally, research is being directed at identifying new proteins in the blood that can detect liver cancer early or predict which patients will develop liver cancer.
 Symptomer på kronisk gastrointestinal blødning
Symptomer på kronisk gastrointestinal blødning
 Hvordan Annas liv ændrede sig:Parasit-IBS-forbindelsen
Hvordan Annas liv ændrede sig:Parasit-IBS-forbindelsen
 Antibiotika som behandling for IBS
Antibiotika som behandling for IBS
 Hvor lang tid tager det at hele fra IBD?
Hvor lang tid tager det at hele fra IBD?
 Anti-coronavirus-molekyler fra mikrober kan være nøglen til nye behandlinger
Anti-coronavirus-molekyler fra mikrober kan være nøglen til nye behandlinger
 Måder til at hjælpe dit barn med at udvikle gode spisevaner
Måder til at hjælpe dit barn med at udvikle gode spisevaner
 Hvor lang tid tager det for en saltvandsskylning at virke?
Det kan tage 30 minutter til en time for en saltvandsskylning at virke som et afføringsmiddel, selvom det i nogle tilfælde kan tage længere tid En saltvandsskyl involverer at drikke varmt vand blande
Hvor lang tid tager det for en saltvandsskylning at virke?
Det kan tage 30 minutter til en time for en saltvandsskylning at virke som et afføringsmiddel, selvom det i nogle tilfælde kan tage længere tid En saltvandsskyl involverer at drikke varmt vand blande
 At drikke kaffe kan forbedre overlevelsesresultaterne for tyktarmskræft
Kaffekop på et træbord. At drikke kaffe, uanset om det er regelmæssigt eller koffeinfrit, kan forlænge overlevelsestiden hos mennesker med tyktarmskræft, foreslår en ny JAMA Oncology-undersøgelse. For
At drikke kaffe kan forbedre overlevelsesresultaterne for tyktarmskræft
Kaffekop på et træbord. At drikke kaffe, uanset om det er regelmæssigt eller koffeinfrit, kan forlænge overlevelsestiden hos mennesker med tyktarmskræft, foreslår en ny JAMA Oncology-undersøgelse. For
 Ernæring og oppustethed:Hvad du behøver at vide
Hos Ignite arbejder vi med en bred vifte af fordøjelsesforstyrrelser, hvor abdominal oppustethed og udspilning er en af de mest almindelige blandt vores kunder. For nogle mennesker sker oppustethed
Ernæring og oppustethed:Hvad du behøver at vide
Hos Ignite arbejder vi med en bred vifte af fordøjelsesforstyrrelser, hvor abdominal oppustethed og udspilning er en af de mest almindelige blandt vores kunder. For nogle mennesker sker oppustethed